In the busy world of healthcare, where every decision matters and every process needs to run smoothly, one big challenge is medical billing. Handling the money side of things while providing care can be tricky. That’s where choosing the right medical billing partner becomes really important.
Picture this: a system where money matters are dealt with smoothly, insurance claims get sorted quickly, and your practice’s income is boosted—all without you having to worry about the nitty-gritty of billing. That’s what a good medical billing partner offers: someone reliable to take care of all the billing stuff, so you can focus on giving top-notch care to your patients.
In this blog, we’ll dive into why medical billing partners are so important and how they can really make a difference for healthcare practices. We’ll talk about what they do, why outsourcing billing tasks is a smart move, and how it can help practices run more smoothly. So, let’s jump in and explore the world of medical billing partners together!
The Role of Medical Billing Partners in Healthcare
In the world of healthcare, medical billing partners are like trusted helpers for medical practices. They’re experts in managing all the ins and outs of medical billing so that practices can focus on taking care of patients.
Basically, a medical billing partner is a company that specializes in handling all the paperwork and processes involved in medical billing for healthcare practices. They take care of things like submitting insurance claims and managing finances. By teaming up with these partners, medical practices can free up their time and energy to focus on what they do best: providing great care to patients.
Services Offered by Medical Billing Partners
Now, let’s take a closer look at some of the services these partners offer.
Claims Submission and Management:
One of the primary responsibilities of a medical billing partner is to handle the submission and management of insurance claims on behalf of the healthcare practice. This includes preparing and submitting claims to insurance companies, tracking claim status, and following up on any denials or rejections.
Payment Posting:
After claims are processed and reimbursements are received, medical billing partners are responsible for accurately recording and posting payments in the practice’s financial system. This involves reconciling payments received from insurance companies, government payers, and patients, ensuring that all transactions are properly accounted for.
Revenue Cycle Management:
Effective revenue cycle management is essential for the financial health of a medical practice. Medical billing partners oversee the entire revenue cycle, from patient registration to final payment. This includes verifying patient insurance coverage, calculating patient responsibility, and ensuring timely and accurate billing and collections.
Coding Assistance:
Medical coding is a critical component of the billing process, as it determines how healthcare services are translated into standardized codes for billing purposes. Medical billing partners provide expert coding assistance to ensure that all services rendered are accurately coded according to industry standards and payer guidelines.
Denial Management:
Despite the best efforts, claim denials are an inevitable part of the billing process. Medical billing partners are equipped to handle denials promptly and effectively, identifying the root causes of denials and taking corrective action to minimize future occurrences. This may involve appealing denials, resubmitting claims with additional documentation, or implementing process improvements to prevent similar issues in the future.
Reporting and Analytics:
In addition to day-to-day billing activities, medical billing partners offer comprehensive reporting and analytics capabilities to help healthcare practices monitor their financial performance and identify areas for improvement. These reports provide valuable insights into key metrics such as reimbursement rates, claim submission efficiency, and revenue cycle trends, empowering practices to make data-driven decisions to optimize their revenue cycle operations.
By leveraging the expertise and resources of a medical billing partner, healthcare practices can streamline their billing processes, improve revenue capture, and enhance overall operational efficiency, ultimately allowing them to focus on what matters most: providing high-quality care to their patients.
Importance of Outsourcing Medical Billing Tasks:
Outsourcing medical billing tasks has become increasingly essential for healthcare practices seeking to thrive in today’s complex healthcare landscape. Here’s why:
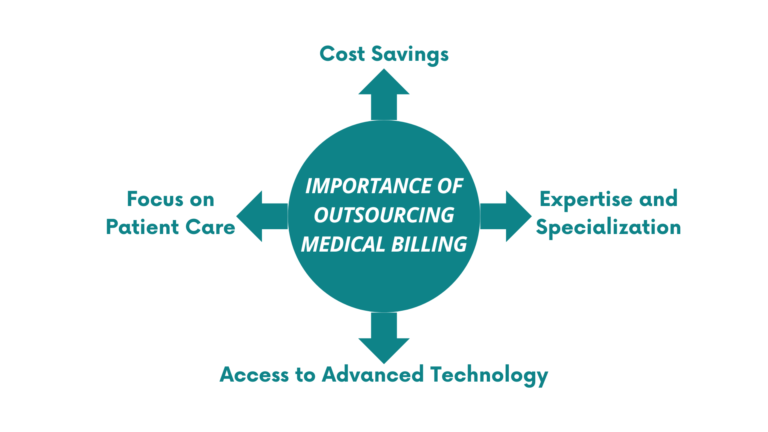
Expertise and Specialization:
Medical billing is a highly specialized field that requires expertise in coding, billing regulations, and payer requirements. By outsourcing billing tasks to a dedicated medical billing partner, practices can leverage the specialized knowledge and experience of professionals who are well-versed in the intricacies of medical billing. This ensures accuracy and compliance in billing processes, reducing the risk of costly errors and claim denials.
Focus on Patient Care:
Managing medical billing in-house can be time-consuming and resource-intensive, diverting valuable time and attention away from patient care. By outsourcing billing tasks to a trusted partner, healthcare providers can free up resources and focus their efforts on delivering high-quality care to their patients. This not only improves patient satisfaction but also enhances overall practice efficiency and productivity.
Cost Savings:
Outsourcing medical billing tasks can result in significant cost savings for healthcare practices. By eliminating the need to hire and train in-house billing staff, invest in billing software and infrastructure, and navigate the complexities of billing regulations, practices can reduce overhead expenses and achieve greater financial efficiency. Additionally, medical billing partners often operate on a fee-for-service basis, allowing practices to scale their billing costs according to their needs and the volume of services rendered.
Access to Advanced Technology:
Medical billing partners invest in advanced technology and software solutions to streamline billing processes and improve efficiency. By partnering with a reputable billing company, practices gain access to cutting-edge billing technology and tools that they may not have the resources to implement or maintain in-house. This technology enables practices to automate routine billing tasks, reduce manual errors, and expedite the claims submission and payment posting process, leading to faster reimbursements and improved cash flow.
Why Choose a Medical Billing Partner?
There are a lot of good reasons to have a medical billing partner rather than doing ̉it in-house. Let us see some of the crucial ones.
Focus on Core Competencies:
Outsourcing billing tasks to a medical billing partner allows healthcare providers to focus on their core competencies: delivering exceptional patient care. By offloading billing responsibilities to a dedicated partner, practices can redirect resources and attention to clinical activities, improving overall practice efficiency and patient satisfaction.
Scalability and Flexibility:
Medical billing partners offer scalable solutions that can adapt to the evolving needs and volume of services provided by healthcare practices. Whether a practice is small or large, a reputable billing company can tailor its services to accommodate fluctuations in workload and ensure consistent revenue flow.
Cost Efficiency:
Partnering with a medical billing company can result in cost savings for healthcare practices. By outsourcing billing tasks, practices avoid the expenses associated with hiring and training in-house billing staff, investing in billing software and infrastructure, and navigating billing regulations independently. Additionally, medical billing partners often operate on a fee-for-service basis, allowing practices to control and manage their billing costs more effectively.
Compliance and Risk Mitigation:
Staying compliant with constantly evolving billing regulations and payer requirements can be challenging for healthcare practices. Medical billing partners have the expertise and resources to navigate these complexities effectively, reducing the risk of costly errors, claim denials, and compliance issues. By partnering with a reputable billing company, practices can mitigate risk and ensure adherence to regulatory standards.
How Medical Billing Partners Can Improve Revenue and Efficiency for Medical Practices:
Let’s explore how medical billing partners can enhance revenue and efficiency for medical practices:
Optimized Claim Submission:
Medical billing partners have expertise in coding, billing regulations, and payer requirements, enabling them to accurately prepare and submit claims on behalf of medical practices. By ensuring that claims are coded correctly and submitted promptly, billing partners maximize the chances of claims being accepted and reimbursed promptly, thus improving revenue flow.
Reduced Claim Denials:
Claim denials can significantly impact practice revenue and cash flow. Medical billing partners employ proactive measures to reduce claim denials, such as thorough claim scrubbing to identify and correct errors before submission, as well as timely follow-up on denied claims to resolve issues promptly. By minimizing claim denials, billing partners help practices maximize revenue capture and reduce revenue leakage.
Efficient Payment Posting:
Medical billing partners handle the timely and accurate posting of payments received from insurance companies and patients. By efficiently reconciling payments with claims and updating the practice’s financial records, billing partners ensure that revenue is accurately recorded and accounted for, improving financial transparency and management.
Streamlined Revenue Cycle Management:
The revenue cycle encompasses the entire process of patient registration, appointment scheduling, claims submission, payment posting, and accounts receivable management. Medical billing partners streamline the revenue cycle by implementing efficient workflows, automating repetitive tasks, and leveraging technology to expedite processes. By optimizing the revenue cycle, billing partners help practices accelerate revenue collection and improve cash flow.
Access to Performance Analytics:
Medical billing partners provide comprehensive reporting and analytics tools that enable practices to track key performance metrics, such as claim submission rates, reimbursement rates, and accounts receivable aging. By analyzing these metrics, practices can identify trends, patterns, and areas for improvement in their revenue cycle operations. Billing partners collaborate with practices to implement data-driven strategies for optimizing revenue generation and operational efficiency.
Compliance Management:
Staying compliant with regulatory requirements and payer guidelines is essential for avoiding penalties and maintaining the integrity of the revenue cycle. Medical billing partners stay abreast of changes in billing regulations and payer policies, ensuring that practices remain compliant with coding and billing standards. By mitigating compliance risks, billing partners help practices avoid costly fines and penalties that could impact revenue and reputation.
The Top 10 Medical Billing Partners in the US

Promantra:
Since its inception in August 2003, Promantra has established itself as a premier provider of healthcare IT services and a trusted medical billing partner, catering to diverse sectors within the healthcare industry. With headquarters in Somerset, New Jersey, and a dedicated delivery center in Hyderabad, India, Promantra has consistently assisted U.S. healthcare providers in operating more efficiently, competing effectively in their markets, and delivering unparalleled patient care.
The Heart of Our Work: Revenue Cycle Management (RCM)
At Promantra, our success and growth revolve around our Revenue Cycle Management (RCM) service. As a leading RCM company, we have significantly contributed to the expansion of our company, enabling us to offer comprehensive support to the healthcare industry. We take pride in our:
Quality Control Framework:
Promantra maintains a rigorous quality control framework to ensure the highest standards in RCM services.
Service Delivery Innovation:
Our commitment to service delivery innovation continually evolves to meet the dynamic needs of our clients and the evolving healthcare landscape.
Commitment to Excellence:
Our primary objective is to empower healthcare practices to achieve their financial goals. We achieve this through innovation, sustained growth, and the utilization of our proprietary technology. We uphold the highest ethical standards, striving to be good corporate citizens in all aspects of our operations.
Our Commitments:
Customer Delight:
We are unwavering in our commitment to ensuring customer delight. We aim to exceed your expectations by delivering exceptional healthcare IT services.
Global Standards Compliance:
Promantra adheres to global standards, including ISO 27001 and ISO 9001, to maintain the highest levels of quality, security, and integrity.
Creating a Knowledgeable Workforce:
We are dedicated to fostering a knowledgeable, committed, and spirited workforce. Our employees are our greatest asset, and we invest in their growth and development.
Invoisync:
Invoisync sets itself apart by leveraging a virtual U.S.-based team seamlessly integrated with clients’ operations to provide comprehensive support and fulfill essential duties. With a collective experience of over 200 years in finance, high-tech, investments, and business, Invoisync is uniquely positioned to cater to diverse needs. Certified by AAPC and compliant with HIPAA regulations, Invoisync demonstrates proficiency in ICD-10 medical coding, ensuring accuracy and compliance in all operations.
Invoisync offers a range of services and features, including authorization request & tracking, electronic & paper claim submission, denial review & management, credentialing, appointment scheduling, prescription processing, payroll services, HR benefits, bank transaction monitoring, and more. With a focus on customization and flexibility, clients can mix and match services to align with their specific needs and preferences.
Invoisync provides custom pricing based on the services required by each client, ensuring cost-effectiveness and scalability. Clients have the flexibility to tailor their service package according to their unique needs, optimizing their investment in healthcare IT services.
At Invoisync, we are committed to delivering exceptional services that exceed our clients’ expectations. With a dedication to innovation, quality, and customer satisfaction, we strive to be a trusted partner in driving success for healthcare practices. Our virtual team approach, combined with our extensive experience and expertise, ensures that clients receive the highest level of support and service excellence.
DrChrono:
DrChrono isn’t just a platform; it’s a comprehensive healthcare ecosystem designed to empower providers of all sizes with seamless integration and innovative solutions. Renowned for its excellence in Electronic Health Records (EHR) and telehealth, DrChrono offers a myriad of services tailored to meet the unique needs of modern medical practices. From large institutions to small clinics, DrChrono’s highly-rated software solutions cater to a diverse clientele, providing a wealth of features designed to streamline workflows and enhance patient care.
At the heart of DrChrono’s offerings lies the fusion of EHR and medical billing, simplifying administrative tasks and maximizing efficiency. With intuitive clinical workflows, robust patient scheduling capabilities, and seamless insurance pre-approval processes, DrChrono empowers providers to focus on what matters most – delivering exceptional care to their patients. The integration of telemedicine capabilities further extends the reach of healthcare services, facilitating remote consultations and enhancing accessibility for patients.
With features like electronic medical records and cloud storage, billing profiles, claim submission to Emdeon, patient statements, HCFA 1500 claim forms, and custom billing codes, DrChrono offers a comprehensive suite of tools to meet the diverse needs of modern medical practices. Whether you’re looking for specialty-specific templates or customizable billing solutions, DrChrono’s offerings are tailored to meet your needs.
DrChrono’s custom pricing in tiered plans ensures flexibility and scalability, allowing practices to choose the solution that best fits their size and location. Whether you’re a small clinic or a large institution, DrChrono’s “all-in-one” approach to medical billing and EHR services makes it a compelling choice for healthcare providers seeking efficiency, innovation, and excellence in today’s dynamic healthcare landscape.
ClaimCare:
In the realm of medical billing, size isn’t everything, and ClaimCare proves this with its remarkable offerings tailored to meet the unique needs of healthcare providers. Despite its smaller stature compared to industry giants, ClaimCare packs a punch with its unparalleled expertise and personalized approach to client satisfaction. With a management team boasting a combined 80 years of experience in medical billing procedures and software applications, ClaimCare is more than equipped to tackle the challenges of modern healthcare administration.
ClaimCare takes pride in its team, meticulously assembled to address clients’ everyday needs with precision and care. With a track record of delivering impressive results, including a 15%-25% increase in collections for clients and maintaining days in AR under 40, ClaimCare is synonymous with excellence in medical billing services.
When it comes to features, ClaimCare doesn’t disappoint. From an instant payment program that allows clients to be paid within 24 hours to pre-approval for claims, analytical patient collection processes, and a revenue denial management system, ClaimCare offers a comprehensive suite of tools to optimize revenue generation and streamline administrative tasks.
With electronic medical records software, dashboard reports, practice analytics, monthly reporting on revenue and other factors, and automated claim tracking, ClaimCare empowers healthcare practices to thrive in today’s competitive landscape.
ClaimCare’s commitment to customer satisfaction is further underscored by its custom pricing model, ensuring that medical practices of all kinds can benefit from its services. Whether you’re a small clinic or a specialized institution, ClaimCare’s personalized approach and robust offerings make it a valuable partner in navigating the complexities of medical billing and practice management.
Advanced Data Systems Corp.:
In the realm of healthcare IT solutions, Advanced Data Systems Corp. stands tall as a trusted partner for practices seeking excellence in software solutions and outsourced medical billing. With a prestigious clientele including Pulmonary and Intensive Care Specialists of New Jersey, Park Avenue Medical Associates, and the Hispanic Counseling Center, Advanced Data Systems Corp. has earned a solid reputation for its commitment to quality and transparency.
One of the hallmarks of Advanced Data Systems Corp. is its unwavering dedication to transparency and accessibility for clients. With the ability to access documents 365 days a year, clients can stay informed about their business’s performance and progress at all times. Moreover, clients praise the company’s responsiveness, with the assurance of being able to reach someone immediately when issues arise, ensuring prompt resolution and peace of mind.
Advanced Data Systems Corp. goes beyond providing software solutions and outsourced billing services; it offers a comprehensive suite of features designed to optimize practice management and revenue generation.
From claim submission and out-of-network alerts when scheduling to automated eligibility verification and denial resubmission within 72 hours, Advanced Data Systems Corp. equips practices with the tools they need to succeed. Additional features such as access to a patient responsibility estimator, a mobile application, reminder texts for payment to patients, a patient billing call center, and robust financial reporting capabilities further enhance practice efficiency and profitability.
With a reported average revenue increase of 10%-20% among customers, Advanced Data Systems Corp. delivers tangible results and drives success for its clients. The provision of a dedicated account manager ensures personalized attention and support, further solidifying the company’s commitment to client satisfaction.
Advanced Data Systems Corp. offers custom pricing for its services, ensuring that each practice receives a tailored solution that meets its unique needs. For those interested, a 2-minute demo is available on the company’s website, providing a glimpse into the innovative solutions and capabilities offered by Advanced Data Systems Corp.
AthenaHealth:
In the world of medical billing and practice management, AthenaHealth stands out for making things easy. They use smart tools to handle claims, solving most issues on the first try with over 23,000 rules. Each year, they check over 400 million claims and collect a whopping $29 billion for their clients. AthenaHealth isn’t just about billing; they offer a whole suite of services like EHR, telehealth, and patient engagement tools.
Some key features include HIPAA-certified medical coding, easy registration and co-pay collection, detailed reports, quick resolution of claim denials, appointment scheduling, reminders, and a complete package called AthenaOne. This includes EHR, patient engagement tools, finances, telehealth, and more.
AthenaHealth offers personalized pricing for its services, and you can easily schedule a one-on-one meeting on its website to learn more about how they can help your business.
Advanced MD:
Advanced MD stands out for its customer-friendly approach, offering enticing features like low upfront costs and no long-term agreements. This flexibility appeals to customers for a couple of reasons. Firstly, it allows them to try outsourced billing with the option to switch if they’re not satisfied. Secondly, for those looking to build their billing department, Advanced MD offers the convenience of outsourcing day-to-day billing operations while they train their staff. This flexibility makes them a versatile solution, whether you’re seeking a short-term or long-term partnership.
Despite their flexibility, Advanced MD doesn’t compromise on features. From comprehensive reporting and analytics to handling appeals and secondary filings, Advanced MD equips businesses with the tools they need to streamline revenue cycle management. Other key features include claim and unpaid claim management, integrated Electronic Health Records (EHR), scheduling, and a user-friendly mobile application.
Advanced MD understands that one size doesn’t fit all when it comes to billing solutions, which is why they provide custom quotes tailored to the unique needs of each business. Whether you’re a small practice or a larger institution, Advanced MD ensures that you receive a solution that aligns with your business size, feature requirements, and contract terms. With the option to easily switch between outsourced or in-house billing, Advanced MD offers the flexibility and support needed to navigate the complexities of medical billing with confidence.
Kareo:
Kareo stands out in the medical health community by offering a wide range of products and services designed to simplify administrative and billing tasks. From telehealth to Electronic Health Records (EHR), Kareo’s software solutions cater to various needs within the healthcare industry. Their outsourcing services are particularly noteworthy, catering to businesses of all sizes and providing access to billing experts dedicated to helping clients navigate the complexities of medical billing.
One of Kareo’s key strengths lies in its approach to outsourcing services. Instead of a one-size-fits-all approach, Kareo matches clients with billing experts who specialize in their specific practice field. With a network of over 1,600 established billing companies, Kareo ensures that clients receive personalized support tailored to their unique needs and requirements.
Kareo’s software features are comprehensive and user-friendly, covering essential functions such as capturing charges at the point of care, scheduling tools, a nationwide billing rules engine, claims management and tracking, billing analytics, and seamless documentation uploading and tracking across teams. With Kareo, healthcare practices can streamline their operations, enhance billing efficiency, and focus on delivering quality care to their patients.
CureMD:
CureMD stands out as one of the most comprehensive and versatile medical billing companies in the US, with expertise spanning over 32 specialties. Leveraging advanced AI technology, CureMD offers a complete revenue cycle management solution for medical practices, ensuring efficiency and accuracy throughout the billing process. With over 20 years of industry experience, customers can trust in CureMD’s commitment to delivering high-quality service and maximizing revenue potential.
CureMD’s extensive range of features and benefits caters to the diverse needs of medical practices, including evaluation and assessment of fee schedules, verification of eligibility, assistance with electronic data interchange (EDI), electronic remittance advice (ERA), and provider enrollment. Additionally, CureMD facilitates the submission of electronic and paper claims, management of accounts receivable, billing of secondary insurance, and handling of incoming patient calls.
With a focus on thorough follow-up and proactive management, CureMD ensures efficient processing of insurance claims and timely reimbursement. Their services extend to recovery of old accounts receivable, notification of referrals and authorizations, entry of charges for all specialties, recording of insurance and patient payments, and processing and mailing of patient statements. Furthermore, CureMD diligently reviews and manages claim denials, providing support for appeals on all claims that have been denied or underpaid.
CareCloud:
At CareCloud, the focus is on providing customers with a personalized and comprehensive revenue cycle management experience, which they aptly term “concierge revenue cycle management.” This approach ensures that all aspects of the billing process are expertly handled, allowing healthcare providers to focus on patient care with confidence. CareCloud offers end-to-end billing services delivered by a specialized team of qualified billers, ensuring efficiency and accuracy throughout the revenue cycle.
Among the standout features and benefits offered by CareCloud are seamless integration or installation of Practice Management (PM) and Electronic Health Records (EHR) systems, ensuring streamlined workflows and enhanced productivity. Customers also benefit from dedicated support staff who are readily available to address any queries or concerns promptly.
CareCloud’s services encompass electronic and paper claims submission, comprehensive claim management, and print and mailing services for clients, simplifying administrative tasks and reducing manual efforts. The platform also facilitates posting of paper remittance, error fixes, and assists in credentialing healthcare providers, ensuring compliance and smooth operations.
Other notable features include benefits verification, an inbound patient call center, and assistance with workers’ compensation claims. With CareCloud, healthcare providers can trust in a reliable and efficient billing solution that caters to their unique needs, allowing them to focus on delivering exceptional care to their patients while enjoying peace of mind knowing that their revenue cycle management is in expert hands.
Summing Up
In conclusion, as you’ve learned about the array of options available in the medical billing landscape, we at Promantra invite you to consider us as your trusted partner in optimizing your revenue cycle management.
With our proven track record, dedication to excellence, and commitment to personalized service, we stand ready to support your practice’s success.
Ready to experience the benefits of partnering with Promantra? Reach out to us today to schedule a personalized consultation.
Let’s discuss how our tailored solutions can streamline your billing processes, maximize revenue, and enhance overall practice efficiency. Don’t miss out on the opportunity to elevate your practice to new heights with Promantra by your side.
Take the next step towards unlocking your practice’s full potential. Contact us now to get started!