Nearly all US healthcare providers have experienced the sinking feeling of encountering a roadblock between themselves and the best course of treatment for their patient. This roadblock, the prior authorization process, often feels like an intricate maze of paperwork and waiting.
A recent American Medical Association (AMA) survey revealed that a whopping 94% of physicians experience delays in patient care due to prior authorization. This translates to frustration for both you and your patients, hindering the efficiency and quality of care delivery.
Understanding the prior authorization process is crucial for navigating the complexities of US healthcare. This multi-step process requires securing approval from a patient’s health plan before administering specific services or medications. While intended to manage costs, prior authorization can create significant administrative burdens for providers, diverting valuable time and resources from direct patient care.
What is Prior Authorization in healthcare?
Prior authorization (PA), also known as precertification, predetermination, or pre-approval, is a multi-step process required by many health insurance plans in the US. It mandates that healthcare providers obtain written approval from a patient’s insurance company before administering specific services or medications. Prior authorization serves as a cost-control mechanism primarily used by Medicaid and other insurers to manage drug expenditures and ensure appropriate medication use. Although it aims to reduce unnecessary costs and improve patient safety, navigating the prior authorization process can be time-consuming and complex for both providers and patients
Importance of Prior Authorization in Healthcare
While prior authorization might seem like an administrative burden, it does hold some benefits for both patients and providers:
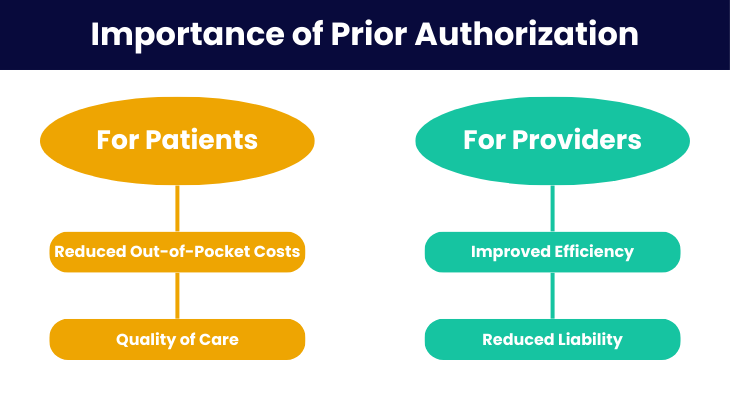
For Patients:
- Reduced Out-of-Pocket Costs: By securing prior authorization beforehand, you can ensure the chosen treatment is covered by the patient’s plan. This minimizes the risk of patients facing unexpected out-of-pocket expenses for services or medications they were unaware wouldn’t be covered.
- Quality of Care: Prior authorization can, in some cases, act as a safeguard against unnecessary or potentially harmful treatments. By requiring justification for certain procedures, it encourages evidence-based medicine and promotes appropriate care.
Real-Life Example:
- A study of 42 patients with inflammatory bowel disease (IBD) found prior authorization delays averaged nearly 6 days, with some waiting up to 34 days. Patients on government health plans faced longer delays, leading to serious health issues.
- A 2023 American Medical Association survey showed nearly a third of doctors reported health problems due to these delays, with many patients abandoning treatment. Faster systems like electronic prior authorization are needed to improve care access.
For Providers:
- Improved Efficiency: A streamlined prior authorization process can help providers obtain timely approvals for necessary treatments, minimizing delays in patient care.
- Reduced Liability: By following the prior authorization process, providers can ensure they are adhering to the terms and conditions of the patient’s insurance plan, potentially reducing the risk of denials or liability issues.
Why Do Health Insurers Require Prior Authorization?
The prior authorization process, while often causing frustration for both providers and patients, serves several key purposes for health insurers. Here’s a breakdown of the primary reason’s health insurers utilize prior authorization:
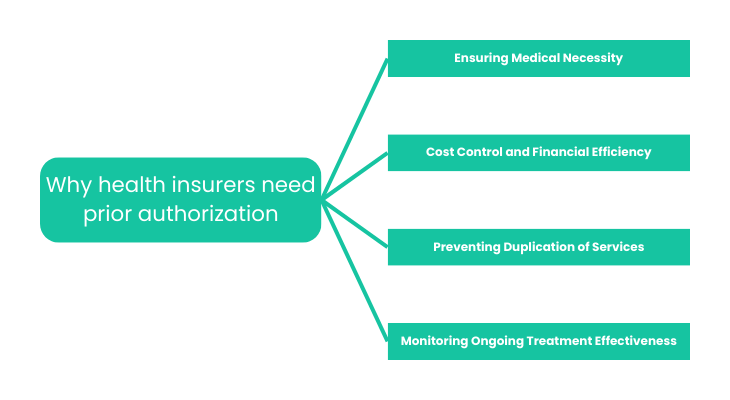
- Ensuring Medical Necessity: At the heart of prior authorization lies the concept of medical necessity. Insurance companies want to ensure the service or medication being requested is truly essential for the patient’s specific condition, based on established medical guidelines and evidence-based practices. They aim to prevent unnecessary healthcare spending on treatments lacking a proven benefit for the patient’s diagnosis.
Example: A doctor might prescribe a powerful pain medication to a patient with a mild backache. Prior authorization allows the insurer to assess if less invasive measures like physical therapy or over-the-counter pain medication would be a more appropriate first-line treatment before approving the stronger medication.
- Cost Control and Financial Efficiency: Healthcare costs continue to rise, and prior authorization acts as a tool for insurers to manage these costs. By evaluating the necessity and cost-effectiveness of proposed treatments, they can potentially steer patients towards more affordable options when equally effective alternatives exist.
Example: A brand-new, high-cost medication might be prescribed for a particular condition. Prior authorization allows the insurer to explore if a generic medication with a proven track record could achieve the same results at a lower cost for the plan.
- Preventing Duplication of Services: With patients potentially seeing multiple healthcare providers, prior authorization helps prevent unnecessary duplication of services.
Example: A patient might be referred to a specialist for a particular condition. Prior authorization allows the insurer to verify if similar tests or procedures haven’t already been performed by another provider within a reasonable timeframe, avoiding unnecessary repetition of services.
- Monitoring Ongoing Treatment Effectiveness: In some cases, prior authorization can be used to monitor the effectiveness of ongoing treatment plans. This is particularly relevant for chronic conditions or treatments requiring long-term use of medications.
Example: A patient with a chronic illness might be on a long-term course of medication. Prior authorization for refills can act as a checkpoint for the insurer to assess if the medication continues to be necessary and effective, potentially prompting a review of the treatment plan if needed.
How Does the Prior Authorization Process Work?
Now that we understand the rationale behind prior authorization, let’s delve into the nitty-gritty of the process itself. Buckle up, because navigating this maze can involve several steps and require clear communication between both healthcare providers and insurance companies. Here’s a breakdown of the typical workflow:
- Initiating the Process:
The prior authorization process starts when a healthcare provider identifies that a patient requires a specific procedure, test, medication, or device. The provider’s staff then reviews the health plan’s policies or formulary to determine if prior authorization is necessary. This process may include:
- Electronically submitting a request: Many insurance companies have online portals where providers can submit prior authorization requests electronically.
- Faxing or mailing a form: In some cases, the insurer might require submitting a paper form outlining the treatment details and justification for medical necessity.
The specific information required for prior authorization requests can vary depending on the insurance company and the service or medication being requested.
However, some common elements might include:
- Patient demographics: Name, date of birth, insurance ID number
- Diagnosis: A clear and concise diagnosis code for the patient’s condition
- Treatment plan: Detailed description of the proposed service or medication, including dosage and duration
- Medical justification: A clear explanation of why the requested treatment is medically necessary and the most appropriate option for the patient’s specific case. This might involve supporting documentation like medical records, test results, or treatment guidelines.
- Documentation is Key:
Gathering and organizing supporting documentation is crucial for a successful prior authorization request. This documentation might include:
- Clinical notes: Detailed notes from the provider outlining the patient’s condition, history, and rationale for the chosen treatment.
- Test results: Relevant lab results, X-rays, or other diagnostic tests supporting the diagnosis and treatment plan.
- Treatment guidelines: References to established medical guidelines or protocols supporting the use of the requested service or medication for the patient’s specific condition.
- Tracking Deadlines:
Prior authorization requests are subject to deadlines set by the insurance company. These deadlines vary depending on the insurer and the type of service or medication being requested. It’s crucial for the provider’s office to track these deadlines and ensure timely submission to avoid delays in care.
- Collaboration is Essential:
While the responsibility for initiating and completing the prior authorization process falls on the provider’s office, clear communication with the patient is also important. Patients should be informed about the request and any potential delays caused by the prior authorization process. Additionally, some insurance companies allow patients to check on the status of their prior authorization requests directly.
The Role of Healthcare Providers:
Healthcare providers play a pivotal role in navigating the prior authorization maze. Their responsibility lies in:
- Identifying services requiring prior authorization: Understanding which services or medications are subject to prior authorization for specific insurance plans.
- Completing the necessary paperwork: Accurately and comprehensively filling out prior authorization requests and gathering supporting documentation.
- Communicating effectively with patients: Keeping patients informed about the process and potential delays caused by prior authorization.
The Role of Insurance Companies:
Insurance companies have the responsibility to:
- Establish clear and transparent guidelines: Providing clear and readily available information on which services require prior authorization and the criteria used for evaluation.
- Streamlining the process: Utilizing efficient electronic systems for submitting and tracking prior authorization requests.
- Providing timely responses: Responding to prior authorization requests within established timeframes to minimize delays in care.
Services and Medications that Need Prior Authorization
Prior Auth specific requirements can vary depending on the insurance plan, some services and medications are more commonly subject to prior authorization than others. Here’s a breakdown of some frequently encountered categories:
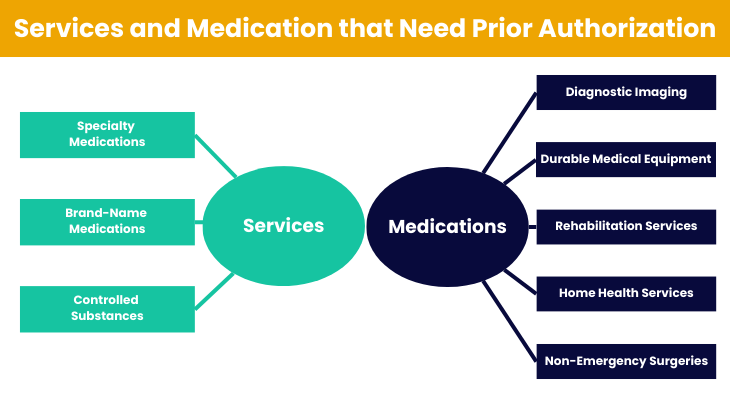
Non-Emergency Services:
Many insurance plans require prior authorization for non-emergency services to ensure medical necessity and cost-effectiveness. Some common examples include:
- Diagnostic Imaging: Advanced imaging tests such as Magnetic Resonance Imaging (MRI), Computed Tomography (CT) scans, and Positron Emission Tomography (PET) scans might require prior authorization, especially if non-invasive alternatives haven’t been explored first.
- Durable Medical Equipment (DME): Items like wheelchairs, hospital beds, and other assistive equipment might require prior authorization to ensure they are medically necessary and appropriate for the patient’s needs.
- Rehabilitation Services: Physical therapy, occupational therapy, and speech therapy services often require prior authorization, particularly when ongoing or long-term treatment plans are recommended.
- Home Health Services: In-home care provided by nurses or other healthcare professionals might require prior authorization, especially if the services are deemed non-essential or custodial in nature.
- Non-Emergency Surgeries: Elective surgeries for cosmetic procedures or non-critical conditions often require prior authorization to ensure they are medically necessary and not purely for aesthetic purposes.
Medications:
Certain medications, particularly those deemed high-cost, brand-new, or with potential for misuse, are more likely to be subject to prior authorization. Here are some common examples:
- Specialty Medications: Drugs used to treat complex or chronic conditions, often carrying a high price tag, might require justification for their use before being approved.
- Brand-Name Medications: While generic alternatives might be available, prior authorization can act as a gatekeeper to ensure the brand-name medication is truly necessary and cost-effective in the patient’s specific case.
- Controlled Substances: Medications with a high risk for abuse or dependence, such as opioids or certain pain medications, often require prior authorization to minimize misuse.
Medications with Potentially Severe Side Effects:
Certain medications, while effective for some conditions, can have serious or life-threatening side effects. Prior authorization helps ensure these medications are used only when absolutely necessary and the potential benefits outweigh the risks. Here are some examples:
- Chemotherapy drugs: Used to treat cancer, these medications can have severe side effects like nausea, hair loss, and damage to healthy cells.
- Immunosuppressant drugs: These medications suppress the immune system to prevent organ rejection after transplants, but can increase the risk of infections.
Medications with High Misuse or Addiction Potential:
Prior authorization helps regulate access to medications with a high potential for misuse or addiction. Here are some examples:
- Opioid pain medications: These powerful pain medications can be highly addictive and prior authorization helps ensure they are prescribed appropriately and only for short-term management of severe pain.
- Stimulants: Used to treat conditions like ADHD, these medications can have side effects like anxiety and insomnia. Prior authorization helps ensure they are prescribed for legitimate medical reasons and not misused.
Cosmetic-Use Drugs:
Many insurance companies exclude coverage for cosmetic procedures and medications used solely for aesthetic purposes. Prior authorization helps ensure these medications are not covered by insurance plans when used for non-medical reasons.
Expensive Drugs with Cheaper Alternatives:
Prior authorization can act as a cost-containment measure by encouraging the use of generic medications or treatments with lower price points. Here are some examples:
- Brand-name medications: When a generic alternative with the same effectiveness exists, prior authorization can help steer patients towards the more affordable option.
- New and emerging medications: High-cost, newly developed medications might require prior authorization to assess their effectiveness and ensure they offer a significant advantage over existing treatments before being routinely covered by insurance.
It’s important to remember that these are just some common examples. The specific medications requiring prior authorization will vary depending on the insurance plan and its guidelines.
Challenges in the Prior Authorization Process
Treatment Delays and Patient Impact:
One of the most significant concerns surrounding prior authorization is the potential for treatment delays. The complex and time-consuming nature of the process can lead to delays in initiating necessary treatments, which can have a detrimental impact on patient outcomes. Here are some ways delays can affect patients:
- Worsening of Conditions: For patients with chronic conditions, delays in receiving medication refills or authorization for ongoing treatment plans can lead to a worsening of their condition.
- Increased Pain and Suffering: For patients requiring pain management or other essential medications, delays in authorization can cause unnecessary pain and suffering.
- Progression of Disease: In some cases, delays in receiving necessary treatment can lead to the progression of a disease, potentially requiring more aggressive and expensive interventions later.
Statistics on Delays and Adverse Effects:
A recent study by the American Medical Association (AMA) found that a staggering 94% of physicians reported experiencing delays in patient care due to prior authorization. This translates to millions of patients potentially facing delays in receiving necessary treatments each year. Additionally, the AMA study found that 24% of physicians reported a serious adverse event for one of their patients due to prior authorization delays, highlighting the potential consequences of these delays for patient safety.
Administrative Burdens on Healthcare Providers:
The prior authorization process can place a significant administrative burden on healthcare providers and their staff. The time and resources spent gathering documentation, completing forms, and following up with insurance companies can detract from the time providers spend directly caring for patients.
Here are some ways the administrative burden affects providers:
- Reduced Patient Care Time: The time spent navigating prior authorization can take away from providers’ time spent seeing patients and delivering care.
- Increased Staff Burnout: The additional workload associated with prior authorization can contribute to staff burnout and decreased morale.
- Higher Costs for Practices: The time and resources dedicated to prior authorization can translate to increased operating costs for healthcare practices.
Controversies and Lack of Transparency:
A major controversy surrounding prior authorization is the lack of clarity and transparency in the criteria used by insurance companies to evaluate requests. This lack of transparency makes it difficult for providers to predict approval outcomes and can lead to frustration and wasted time. Additionally, some argue that the emphasis on cost-containment through prior authorization can sometimes supersede patient needs, leading to denials for essential treatments.
Moving Forward: Addressing the Challenges
While prior authorization can serve a purpose, its current implementation creates significant challenges for both providers and patients. In the next section, we’ll explore some strategies and practical tips to streamline the prior authorization process and ensure timely care for patients.
Strategies for Navigating the Prior Authorization Process
The complexities of prior authorization can feel overwhelming for both providers and patients. However, by employing some strategic approaches, we can navigate this maze more efficiently. Let’s explore some helpful tips:
Strategies for Patients:
- Open communication with healthcare providers: Patients play a crucial role in navigating prior authorization. Open communication with your healthcare provider is essential. Here’s how patients can contribute:
- Discuss potential prior authorization needs with your provider in advance of any procedures or medications being prescribed.
- Understand why a specific treatment might require prior authorization and the rationale behind it.
- Ask your provider for clear explanations and estimated timelines regarding the prior authorization process.
- Maintain organized medical records: Having all your medical records readily available can simplify the process. This includes:
- Insurance information (plan details, ID number)
- Medical history documents
- Past test results and diagnostic reports
- Prescriptions and medication lists
- Documentation of prior treatments and their outcomes
- Understanding Insurance Requirements: Familiarize yourself with the basics of your insurance plan and its prior authorization policies. Here’s what you can do:
- Review your insurance plan documents or contact your insurance company to understand which services or medications might require prior authorization.
- Ask your insurance company about specific requirements for submitting prior authorization requests.
- Inquire about the availability of online portals or resources for tracking the status of your prior authorization requests.
By following these tips, patients can become active participants in navigating prior authorization and ensuring timely access to necessary care.
Tips for healthcare providers:
The prior authorization maze can be particularly challenging for healthcare providers and their staff. However, by implementing some effective strategies, you can streamline the process and minimize disruptions to patient care. Here are some key tips:
Staying Informed:
- Clinical Guidelines and Insurance Policies: Knowledge is power! Staying updated on the latest clinical guidelines for specific conditions and the evolving prior authorization policies of different insurance companies is crucial. This allows providers to anticipate which services or medications might require authorization and tailor their treatment plans accordingly.
- Subscribe to updates and resources from relevant medical associations and professional societies.
- Regularly review your contracts and communication materials from insurance companies to stay informed about changes in prior authorization requirements.
Streamlining Workflow:
- Dedicated Staff: Consider designating a staff member or team specifically responsible for handling prior authorization requests. This dedicated focus can improve efficiency and ensure tasks are completed accurately and promptly.
- Train your designated staff on the intricacies of prior authorization processes for various insurance companies.
- Invest in technology solutions that can automate certain aspects of prior authorization tasks, such as electronic submission of requests and tracking of deadlines.
Effective Documentation:
- Clear and Concise Communication: When completing prior authorization requests, prioritize clear and concise communication. Ensure all necessary information is included, such as:
- A detailed explanation of the patient’s diagnosis and medical necessity for the requested service or medication.
- Supporting documentation like relevant medical records, test results, and treatment guidelines.
- Accurate and up-to-date patient demographics and insurance information.
- Standardization and Templates: Develop standardized templates and protocols for completing prior authorization requests for common scenarios. This can save time and ensure consistency in documentation.
- Maintain a System for Tracking: Implement a system for tracking the status of prior authorization requests for each patient. This allows for proactive follow-up with insurance companies if necessary and helps avoid delays in care.
By following these strategies, healthcare providers can equip their teams to navigate the prior authorization maze more efficiently.
What to Do If Your Prior Authorization Request Is Denied
Even with the best efforts, prior authorization requests can sometimes be denied by insurance companies. While frustrating, it’s important not to give up hope. Here’s a breakdown of what to do if your prior authorization request is denied:
Understanding the Denial:
- Requesting the Reason for Denial: The first step is to understand the specific reason for the denial. This information should be provided by your insurance company, either through an explanation of benefits (EOB) document or by contacting them directly. Common reasons for denial might include:
- Lack of medical necessity: The insurer might not believe the requested service or medication is truly necessary for your specific condition.
- Missing or incomplete information: The submitted documentation might be lacking crucial details or supporting evidence.
- Treatment guidelines not followed: The requested treatment might not align with established medical guidelines for your diagnosis.
- Alternative options available: The insurer might suggest exploring less expensive or less invasive treatment options before approving the requested service.
Appealing the Denial:
Most insurance companies provide an appeals process for denied prior authorization requests. This typically involves submitting a formal appeal with additional information to support your case.
Steps to a Successful Appeal:
- Reviewing and Correcting Paperwork: Carefully review the initial request and supporting documentation to identify any errors or omissions that might have contributed to the denial.
- Providing Additional Evidence: Gather additional documentation to strengthen your case. This could include:
- Updated medical records or test results
- Letters of support from specialists or consulting physicians
- Peer-reviewed medical literature supporting the medical necessity of the requested treatment
- Communicating Effectively: Work closely with your healthcare provider to draft a clear and concise appeal letter. The letter should:
- Briefly restate the patient’s condition and diagnosis.
- Clearly explain why the requested service or medication is medically necessary and the most appropriate course of treatment for the patient.
- Address the specific reasons for the original denial, if available.
- Attach all relevant supporting documentation.
- Following Up: Be proactive and follow up with your insurance company regarding the status of your appeal.
Collaboration is Key:
Open communication and collaboration between you, your healthcare provider, and the insurance company are crucial for a successful appeal. Your provider can advocate for the medical necessity of the treatment and provide additional clinical justification for the appeal.
Additional Resources:
Several resources can offer guidance and support throughout the prior authorization process:
- Your Healthcare Provider: Your provider’s office can assist with completing prior authorization requests, gathering documentation, and navigating the appeals process.
- Your Insurance Company: Most insurance companies have resources available online or through customer service representatives to explain their prior authorization policies and appeals procedures.
- Patient Advocacy Groups: Patient advocacy groups can offer support and guidance specific to your condition and may have resources related to navigating prior authorization denials.
Remember, prior authorization denials can be frustrating, but with the right approach and collaboration, you can often navigate the appeals process and secure the necessary approval for your healthcare needs.
The Future of Prior Authorization
The current state of prior authorization, while intended for cost-containment, can create significant burdens for both patients and providers. However, the tides might be shifting. Here’s a look at recent developments and proposed changes aimed at streamlining the prior authorization process:
Recent Regulatory Changes:
- The Centers for Medicare & Medicaid Services (CMS) Final Rule: In January 2024, CMS implemented a final rule aimed at improving the efficiency and transparency of prior authorization for Medicare Advantage plans. This rule includes provisions such as:
- Standardized Deadlines: Setting standard timeframes for insurance companies to respond to prior authorization requests (72 hours for urgent requests and 7 days for standard requests).
- Electronic Prior Authorization: Encouraging the use of electronic systems for submitting and tracking prior authorization requests.
- Clear Denial Reasons: Requiring insurance companies to provide clear and specific reasons for denying prior authorization requests.
Proposed Reforms and Industry Initiatives:
- Standardized Forms and Processes: Several organizations are advocating for the development of standardized forms and processes for prior authorization requests across different insurance companies. This would simplify the process for providers and reduce errors.
- Real-Time Decisions: The use of advanced technology and data analytics is being explored to enable real-time decisions on prior authorization requests, potentially minimizing delays in care.
- Focus on Patient Outcomes: A shift in focus towards measuring the impact of prior authorization on patient outcomes is gaining traction. This could lead to more emphasis on the medical necessity of treatments and less on purely cost-saving measures.
The Potential Impact:
These changes and proposed reforms hold promise for a more streamlined and efficient prior authorization process. Here’s how these advancements might impact patients and providers:
- Reduced Delays in Care: Faster turnaround times for prior authorization decisions could lead to quicker access to necessary treatments for patients.
- Decreased Administrative Burden: Standardized processes and electronic systems could free up valuable time for providers, allowing them to focus on direct patient care.
- Improved Transparency: Clearer communication regarding denial reasons and standardized criteria for approvals could improve overall transparency in the process.
The Road Ahead:
While the future of prior authorization remains uncertain, recent developments and ongoing discussions indicate a potential move towards a more patient-centered and efficient system. It’s important to stay informed about these changes and advocate for reforms that prioritize timely access to quality care for all.
Streamlining Prior Authorization with ProMantra
The complexities of prior authorization can leave healthcare providers feeling overwhelmed and bogged down by administrative tasks. At ProMantra, we understand the challenges you face and are dedicated to helping you navigate the maze of prior authorization efficiently.
We’ve seen firsthand the negative impact that prior authorization delays can have on patient care. That’s why we offer a comprehensive suite of prior authorization services designed to streamline the process and minimize disruptions to your workflow.
Here’s how ProMantra can empower you:
- Our team of experts stays up-to-date on the latest insurance guidelines and regulations, ensuring your prior authorization requests are completed accurately and meet all necessary criteria.
- We leverage advanced technology to automate tasks and expedite communication with insurance companies, reducing turnaround times and minimizing delays.
- Our focus on clear and concise communication ensures your requests are well-supported with the right documentation, maximizing the chances of first-pass approval.
By outsourcing your prior authorization needs to ProMantra, you can free up valuable time and resources to focus on what matters most – delivering high-quality care to your patients.
To learn more about Promantra’s RCM offerings, contact us today.
Reference: