Medical coding plays a pivotal role in ensuring that patient information is accurately documented and billed. Understanding the different types of medical coding is essential for healthcare professionals, coders, and even patients who want to grasp how their medical data is handled. This blog will delve into the three primary types of medical coding: diagnostic coding, procedural coding, and revenue cycle coding, each serving a distinct function within the healthcare system.
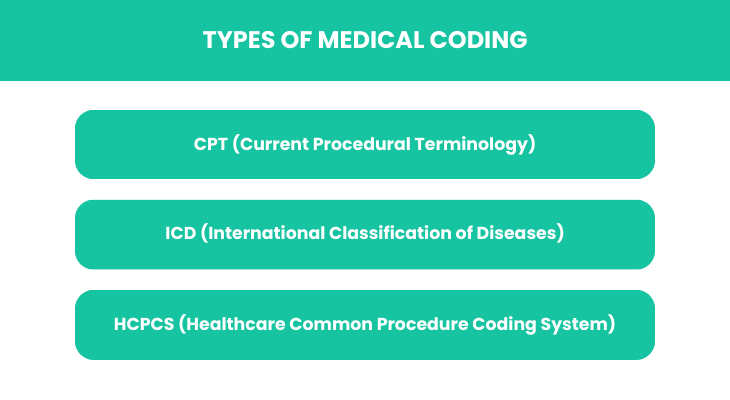
Additionally, we will explore what are the four types of medical coding systems, shedding light on the frameworks that underpin these coding practices, including ICD, CPT, HCPCS, and others. By the end of this blog, readers will have a comprehensive understanding of the various types of medical coding and their significance in the healthcare industry, empowering them to navigate medical documentation with greater clarity.
Whether you are a seasoned professional or someone new to the field, grasping these concepts is crucial for effective communication and operational efficiency in healthcare settings. Join us as we break down medical coding and elucidate its importance in delivering quality patient care.
Types of Medical Coding:
Medical coding is essential for accurately documenting healthcare services, procedures, and diagnoses. The three main types of medical coding include diagnostic coding, procedural coding, and revenue cycle coding. Diagnostic coding focuses on identifying and classifying diseases and conditions, using codes from systems like ICD-10.
Procedural coding, often derived from CPT codes, details the services provided to patients, including surgeries and examinations. Revenue cycle coding integrates both diagnostic and procedural codes to facilitate billing and reimbursement processes. Understanding these types enables healthcare professionals to ensure compliance, maintain accurate records, and improve the overall efficiency of healthcare delivery.
CPT (Current Procedural Terminology):
Current Procedural Terminology (CPT) is a standardized coding system created and maintained by the American Medical Association (AMA). It provides a comprehensive set of codes that represent medical, surgical, and diagnostic services. CPT codes are essential for billing and reimbursement purposes, helping to streamline communication between healthcare providers, insurers, and patients.
This coding system is updated annually to reflect advancements in medical technology and practices. By utilizing CPT, healthcare professionals can ensure accurate documentation of services rendered, which is crucial for billing accuracy and quality patient care. CPT codes play a vital role in maintaining the integrity of healthcare data.
- Description and Purpose: The primary purpose of CPT codes is to provide a uniform language for describing medical services and procedures. Each code corresponds to a specific service, allowing healthcare providers to communicate effectively with insurers and other entities involved in patient care. By using a standardized coding system, CPT facilitates accurate billing, reduces errors, and enhances the efficiency of healthcare operations. Additionally, CPT codes are instrumental in data collection and analysis, enabling researchers and policymakers to track healthcare trends and outcomes. Overall, the description and purpose of CPT codes extend beyond billing; they are fundamental to ensuring quality and transparency in healthcare delivery.
- Common Applications in Healthcare: CPT codes are widely used across various healthcare settings, including hospitals, outpatient clinics, and private practices. They serve as the foundation for billing procedures, enabling healthcare providers to submit claims for reimbursement from insurance companies. CPT codes are also employed in electronic health records (EHRs) to document the services provided to patients accurately. Furthermore, CPT coding is crucial for quality reporting initiatives, as many healthcare organizations use these codes to track performance metrics and patient outcomes. In research, CPT codes help in analyzing healthcare utilization and costs, providing valuable insights for improving healthcare systems and policies.
ICD (International Classification of Diseases)
The International Classification of Diseases (ICD) is a comprehensive coding system developed by the World Health Organization (WHO) to classify and monitor diseases, disorders, and health-related issues globally. It serves as a vital tool for healthcare providers, insurers, and researchers, facilitating accurate diagnosis documentation and statistical analysis. The ICD is regularly updated to reflect advances in medical knowledge, ensuring that healthcare data remains relevant and useful for improving patient care and health policies.
- Overview of Diagnostic Coding: Diagnostic coding involves assigning standardized codes to patient diagnoses and conditions, allowing for consistent communication across the healthcare system. This process is essential for accurate billing, medical record keeping, and health data analysis. By utilizing systems like ICD, healthcare professionals can ensure that diagnoses are documented precisely and uniformly, which aids in treatment planning, reimbursement processes, and public health reporting. Ultimately, effective diagnostic coding enhances patient care and supports healthcare operations.
- Differences Between ICD-9 and ICD-10: The transition from ICD-9 to ICD-10 marked a significant upgrade in diagnostic coding standards. ICD-9 contained approximately 13,000 codes, while ICD-10 expanded this number to over 68,000 codes, allowing for greater specificity and detail in documenting patient diagnoses. Additionally, ICD-10 introduced alphanumeric codes, enhancing flexibility and accommodating new medical knowledge. This transition improved data accuracy, facilitating better patient care, research, and public health initiatives by providing a clearer understanding of health trends and outcomes.
HCPCS (Healthcare Common Procedure Coding System)
The Healthcare Common Procedure Coding System (HCPCS) is a standardized coding system used in the United States to describe healthcare procedures, services, and equipment. It consists of two levels: Level I codes are based on the Current Procedural Terminology (CPT) codes, while Level II codes cover non-physician services and items not included in CPT. HCPCS plays a crucial role in billing, reimbursement, and ensuring uniformity in healthcare communication and data reporting.
- Explanation of Levels I and II: HCPCS is divided into two distinct levels. Level I codes, also known as CPT codes, are numeric codes that represent medical procedures and services performed by healthcare professionals. Level II codes are alphanumeric and used to identify non-physician services, such as durable medical equipment, prosthetics, and ambulance services. Together, these levels provide comprehensive coverage for all healthcare services, ensuring accurate billing and effective communication across various healthcare settings.
- Role in Medical Equipment and Services: HCPCS codes play a vital role in the classification and billing of medical equipment and services. Level II codes specifically identify durable medical equipment, supplies, and other non-physician services, allowing providers to bill Medicare and other insurers accurately. This coding system ensures that patients receive the necessary equipment, such as wheelchairs and oxygen supplies, while facilitating proper reimbursement for healthcare providers. Ultimately, HCPCS enhances the efficiency of healthcare delivery and patient care management.
Other Types of Medical Coding & Its Applications:
In addition to the primary coding systems, various types of medical coding exist to address specific healthcare needs. These include coding for outpatient services, laboratory tests, and anaesthesia coding. Each type serves a unique purpose, ensuring that all aspects of patient care are accurately documented and billed. Additionally, specialty-specific codes allow for more detailed reporting, improving data collection and analysis, which ultimately enhances patient care and operational efficiency within healthcare facilities.
- Revenue Cycle Management (RCM): Revenue Cycle Management (RCM) is a comprehensive process that oversees the financial aspects of healthcare services, from patient registration to billing and collection. RCM optimizes workflows, reduces claim denials, and ensures timely reimbursement for services provided. By effectively managing the revenue cycle, healthcare organizations can enhance cash flow and financial performance. Moreover, RCM practices contribute to improved patient satisfaction by streamlining billing processes and ensuring transparent communication regarding payment responsibilities and options.
- Modifiers and Their Significance: Modifiers are essential components in medical coding that provide additional context to procedure codes, indicating variations in service delivery. They clarify circumstances, such as whether a procedure was altered, performed bilaterally, or was a repeat service. By incorporating modifiers, healthcare providers can enhance the accuracy of claims submitted to insurers. This specificity helps prevent claim denials and ensures appropriate reimbursement, ultimately improving the financial health of healthcare facilities and supporting effective patient care delivery.
The Importance:
CPT Coding: How It Improves Billing Accuracy: CPT coding significantly enhances billing accuracy by providing a standardized language for describing medical procedures and services. This uniformity reduces the risk of errors in claims submission, ensuring that healthcare providers receive appropriate reimbursement for services rendered. Accurate CPT coding also aids in effective communication between providers and insurers, facilitating quicker claim processing. Ultimately, improved billing accuracy leads to better revenue cycle management and contributes to the financial stability of healthcare organizations.
ICD Coding: Importance in Patient Diagnosis and Epidemiology: ICD coding is crucial for accurately diagnosing patients and tracking epidemiological data. By classifying diseases and health conditions, ICD codes enable healthcare providers to document patient diagnoses consistently, which is essential for treatment planning and quality care. Additionally, ICD codes facilitate public health reporting, allowing researchers and policymakers to analyze disease trends, monitor outbreaks, and allocate resources effectively. This comprehensive data collection is vital for improving healthcare quality and addressing public health challenges.
HCPCS Coding: Role in Outpatient Services: HCPCS coding plays a vital role in outpatient services by providing a standardized coding system for non-physician services and medical supplies. This coding ensures accurate billing for various outpatient procedures, durable medical equipment, and ancillary services, allowing providers to receive proper reimbursement. Furthermore, HCPCS codes enhance communication between healthcare providers and insurers, facilitating streamlined claims processing. By improving billing accuracy and efficiency, HCPCS coding ultimately supports the delivery of high-quality outpatient care.
RCM: Enhancing Financial Performance for Healthcare Providers: Revenue Cycle Management (RCM) is essential for enhancing the financial performance of healthcare providers. By optimizing the financial processes from patient registration to billing and collections, RCM improves cash flow and reduces the rate of claim denials. Effective RCM practices help identify revenue opportunities, streamline administrative workflows, and enhance patient satisfaction through clear billing communication. Ultimately, robust RCM enables healthcare organizations to maintain financial stability, invest in quality care, and sustain operational growth.
Conclusion:
Medical coding and revenue cycle management are critical components of the healthcare system that contribute to the accuracy, efficiency, and financial stability of healthcare organizations. Various coding types, including CPT, ICD, HCPCS, and the use of modifiers, ensure that healthcare services are documented and billed accurately. These systems not only facilitate proper reimbursement but also enhance communication among providers, insurers, and patients, which is essential for delivering quality care.
Moreover, effective Revenue Cycle Management (RCM) optimizes financial processes, minimizes claim denials, and improves cash flow, ultimately supporting the operational growth of healthcare facilities. By leveraging comprehensive coding systems and robust RCM practices, healthcare providers can enhance patient outcomes while maintaining financial viability, thereby fostering a healthier community overall.
Promantra’s medical coding expertise empowers practices and hospitals by ensuring timely claims processing and payment. With a dedicated team of certified coders, Promantra enhances billing accuracy and optimizes revenue cycles, minimizing denials. For reliable support in medical coding and efficient claim management, contact Promantra today to streamline your healthcare operations.
Promantra specializes in medical coding solutions that help healthcare practices and hospitals secure timely payments for their services. By leveraging industry expertise and advanced coding techniques, Promantra ensures accurate claims submission and reduces the likelihood of denials.
Reach out to Promantra for tailored coding support and improve your financial performance.