A busy healthcare provider often struggles in documenting every detail during a busy clinic day. In today’s complex healthcare landscape, ensuring efficient medical billing practices is no longer optional – it’s essential. Medical billing practices encompass the entire process of coding services rendered, submitting claims to insurance companies, and collecting patient payments. Streamlining these processes leads to numerous benefits for both healthcare providers and patients.
Why Efficiency Matters
Imagine a scenario where medical billing is plagued by delays and errors. Claims get denied, reimbursements are slow, and patient bills are inaccurate. This not only creates a financial burden for the practice, but also leads to frustration and confusion for patients. Conversely, efficient medical billing practices contribute to a smoother financial flow, allowing healthcare providers to focus on what matters most – delivering quality patient care. For patients, clear and accurate billing improves their financial understanding and overall healthcare experience. This blog will delve deeper into the world of medical billing practices, exploring key components, best practices, and regulations to implement efficient and compliant billing practices.
Understanding the Complexity of Medical Billing
Medical billing might appear simple: a patient receives care, a bill is generated, and payment is collected. However, the process involves intricate details and regulations.
Key Challenges:
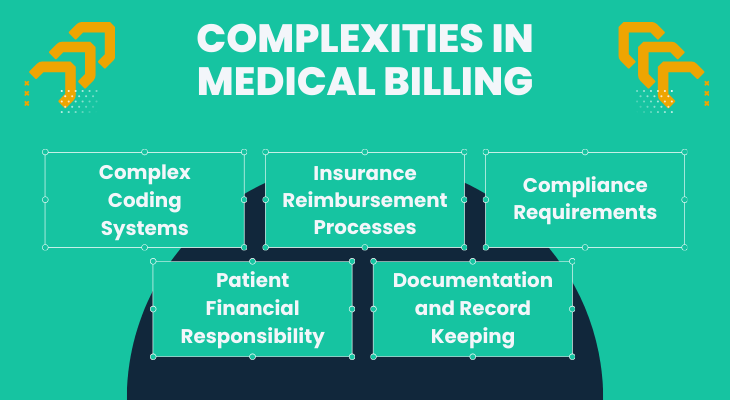
- Complex Coding Systems: Accurately translating medical services into specific codes is crucial for proper reimbursement. The two main coding systems are:
- Current Procedural Terminology (CPT codes): These codes define specific medical services and procedures performed by a healthcare provider.
- International Classification of Diseases, Tenth Revision (ICD-10 codes): These codes classify diagnoses and medical conditions a patient presents with.
- Healthcare Common Procedure Coding System (HCPCS) codes are used for specific services, supplies, and equipment not covered by CPT codes.
- Current Procedural Terminology (CPT codes): These codes define specific medical services and procedures performed by a healthcare provider.
- Insurance Reimbursement Processes: Each insurance company has its own set of rules for covered services and reimbursement rates. Understanding these complexities is essential for submitting accurate claims and maximizing reimbursements.
- Compliance Requirements: A network of federal and state regulations governs medical billing practices. HIPAA safeguards patient privacy, while specific guidelines dictate coding, documentation, and claims submission procedures. Staying compliant is essential to avoid penalties and ensure smooth claim processing.
- Patient Financial Responsibility: Patients often have deductibles, co-pays, and co-insurance to consider. Understanding these concepts and explaining them clearly to patients is crucial to avoid billing disputes and maintain positive relationships.
- Documentation and Record Keeping: Detailed and accurate medical records are the foundation of efficient medical billing. These records should clearly document the patient’s condition, services provided, and the medical necessity for those services. Proper record keeping strengthens the validity of claims and facilitates a smooth billing process.
The Road to Efficiency:
The complexities of medical billing can be daunting. However, by understanding these core elements, healthcare providers can streamline their billing processes and achieve greater efficiency.
Challenges in Medical Billing Practices
Even the most well-run medical practices can face hurdles in managing their billing processes. These challenges can impede efficiency and hinder financial performance. Here’s a closer look at some common issues:
Common Challenges in Medical Billing:
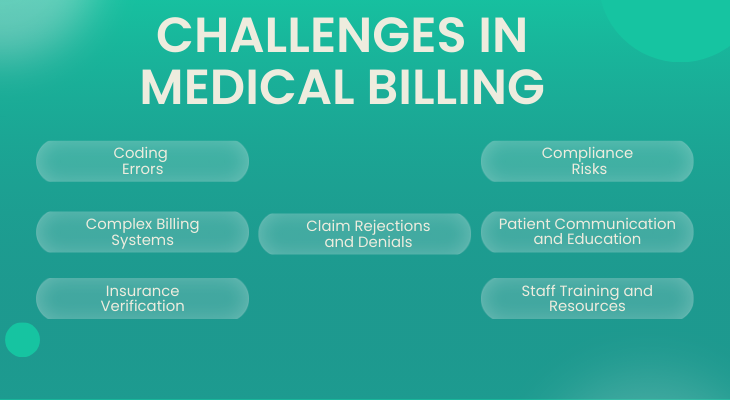
- Coding Errors: Medical coding is a meticulous task. Even minor errors in CPT®, ICD-10, or HCPCS coding can lead to claim denials and lost revenue. Staying up-to-date on coding guidelines and implementing robust quality checks are crucial for mitigating these errors.
- Complex Billing Systems: Mastering the functionalities of your chosen medical billing software is essential for accurate and efficient claim submission. Proper system configuration can streamline workflows and minimize errors.
- Insurance Verification: Verifying patient insurance eligibility and benefits upfront can prevent delays and denials. However, this process can be complex due to ever-changing insurance plans. Regular communication with insurance companies is essential for staying informed.
- Claim Rejections and Denials: Understanding the reasons for claim rejections and denials is vital for maximizing reimbursements. Rejected claims never reach the insurance company and require resubmission. Denied claims are returned unpaid, often requiring an appeals process.
- Compliance Risks: Failure to comply with HIPAA regulations or other billing guidelines can result in hefty fines and penalties. Staying informed about regulatory updates and implementing robust compliance measures is essential for protecting your practice.
- Patient Communication and Education: Patients often struggle to understand complex medical bills. Proactive communication from the practice, explaining billing procedures and patient responsibility in clear language, can foster trust and minimize billing disputes.
- Staff Training and Resources: A well-trained and knowledgeable staff is essential for efficient medical billing. Investing in ongoing training on coding, claims submission, and compliance can yield significant returns on investment.
The Importance of Optimized Medical Billing Practices
Streamlining your medical billing processes can unlock a multitude of benefits that empower your practice to deliver quality care and achieve financial stability. Here’s how optimized billing can contribute to your practice’s success:
Benefits of Optimization:
- Increased Revenue: Efficient billing ensures accurate coding and claim submission, leading to higher acceptance rates and maximized reimbursements from insurance companies. This translates directly to increased revenue for your practice.
- Improved Cash Flow: Faster claim processing and fewer denials mean quicker access to your hard-earned revenue. This improved cash flow allows you to reinvest in your practice, expand services, and ultimately provide better care for your patients.
- Enhanced Patient Experience: Clear, accurate, and timely billing fosters trust with your patients. Reduced confusion and frustration regarding medical bills contribute to a more positive overall patient experience.
- Ensured Compliance: Optimized billing processes help you stay on top of ever-evolving regulations like HIPAA and ensure proper documentation for claim justification. This minimizes the risk of costly penalties and audits.
- Reduced Administrative Burden: A well-oiled billing system frees up valuable staff time previously spent chasing down missing information, correcting errors, and appealing denials. This allows your staff to focus on what matters most – delivering exceptional patient care.
- Enhanced Practice Efficiency: Streamlined workflows and automated processes contribute to a more efficient practice overall. This frees up resources and allows your team to operate at their full potential.
- Promoted Business Growth: By maximizing revenue, improving cash flow, and enhancing patient satisfaction, optimized billing practices contribute significantly to the overall growth and prosperity of your medical practice.
Investing in Efficiency:
Optimizing medical billing requires a strategic approach. Here are some key areas to consider for streamlining your billing processes and improving efficiency:
- Investing in Staff Training: A well-trained billing staff can significantly improve accuracy, reduce errors, and ensure timely claim submission.
- Optimizing Technology and Automation: Consider implementing medical billing software that automates tasks, reduces manual data entry, and streamlines workflows.
- Regular Audit and Compliance Reviews: Staying on top of coding and billing regulations is essential. Regular audits can help identify areas for improvement and ensure compliance with HIPAA and other guidelines.
By investing in these areas, you can achieve a more efficient billing system that maximizes revenue, improves cash flow, and reduces administrative burdens. This allows your practice to focus on what matters most – delivering high-quality patient care.
Key Factors Influencing Medical Billing Efficiency
New regulations, coding updates, and healthcare trends all play a role in shaping medical billing practices. In this final section, we’ll explore some key factors that significantly influence efficiency:
1. Impact of the Affordable Care Act (ACA) on Medical Billing Practices:
The Affordable Care Act (ACA) has had a profound impact on the healthcare industry, including medical billing. Here’s a closer look:
- Increased Patient Volume: The ACA has expanded health insurance coverage, leading to a rise in the number of insured patients. This translates to higher billing volume for medical practices, necessitating efficient processes to handle the increased workload.
- Focus on Preventive Care: The ACA emphasizes preventive care, leading to more coding for screenings and wellness visits. Practices need to adapt their billing systems to capture these services accurately.
- Emphasis on Quality and Value: The ACA incentivizes quality care and value-based payments. Medical billing systems need to be able to track and report on quality metrics to ensure proper reimbursement.
2. Significance of Accurate ICD-10 Coding in Medical Billing Processes:
The transition to ICD-10 coding in 2015 brought a new level of complexity to medical billing. Here’s why accurate ICD-10 coding is crucial:
- Specificity and Detail: ICD-10 codes are more specific than their ICD-9 predecessors. This increased specificity allows for more precise diagnoses, leading to more accurate claim submission and higher reimbursement rates.
- Risk of Denials: Inaccurate ICD-10 coding can lead to claim denials. Investing in proper training and robust coding practices is essential to avoid these costly setbacks.
- Data-Driven Insights: Accurate ICD-10 coding provides valuable data on patient diagnoses. This data can be used to improve population health management and identify areas for cost-reduction.
3. Influence of Consumer-Driven Health Plans (CDHPs) on Medical Billing Efficiency:
Consumer-driven health plans (CDHPs) are a growing trend in healthcare. Here’s how CDHPs influence medical billing:
- Increased Patient Responsibility: With CDHPs, patients have a greater financial stake in their healthcare costs. This necessitates clear and transparent billing practices to empower patients to make informed decisions.
- Focus on Cost Transparency: CDHPs require clear pricing information for medical services. Practices need to ensure their billing systems can generate accurate and easily understandable patient statements.
- Shift Towards Preventive Care: CDHPs often incentivize preventive care to minimize overall healthcare costs. Practices need to adapt their billing processes to capture and bill for preventive services effectively.
Optimizing for the Future:
Recognizing the importance of staying ahead of the curve in medical billing and by understanding these key factors and implementing best practices, medical practices can ensure efficient and compliant billing processes in a constantly evolving healthcare landscape.
Partnering with Us:
Optimizing medical billing can be a complex and ever-changing landscape. Consider partnering with a reputable medical billing service to:
- Navigate Regulatory Complexities: Stay up-to-date on evolving regulations like the Affordable Care Act (ACA) and ensure your practice adheres to the latest coding standards like ICD-10.
- Embrace Efficiency: Leverage a partner’s expertise in streamlining workflows, automating tasks, and implementing best practices to maximize efficiency.
- Adapt to Changing Market Dynamics: The healthcare landscape constantly evolves, with new insurance plans like Consumer-Driven Health Plans (CDHPs) emerging. A partner can help you stay informed and adapt your billing practices accordingly.
By partnering with a qualified medical billing service, you can free up valuable time and resources within your practice, allowing you to focus on what matters most – providing exceptional patient care and achieving long-term financial stability.
Strategies for Optimizing Your Medical Billing Practices
A streamlined medical billing process is the backbone of a financially healthy practice. Beyond the theoretical benefits, let’s delve into practical strategies that can directly strengthen your cash flow and fuel your practice’s growth.
Strategies for Success:
Strengthening Cash Flow Opportunities:
- Prioritize Accurate Coding: Investing in proper coder training and robust quality checks minimizes errors and maximizes claim acceptance rates. This translates directly to faster reimbursements and improved cash flow.
- Embrace Automation: Leverage technology to automate repetitive tasks like claim submission, eligibility verification, and payment posting. This frees up staff time to focus on higher-value activities and expedites the billing process.
- Implement Denial Management Strategies: Develop a system for promptly addressing claim denials and appeals. Proactive follow-up ensures you recoup lost revenue and minimize future denials.
- Offer Flexible Payment Options: Provide patients with various payment options, such as online portals, credit card processing, and installment plans. This flexibility encourages prompt payment and reduces outstanding receivables.
Attracting and Retaining Patients for Follow-Up Visits:
- Prioritize Clear Communication: Ensure patients receive clear and concise explanations of their bills. This fosters trust and reduces billing disputes, encouraging patients to return for future care.
- Offer Appointment Reminders: Implement automated appointment reminders via text or email. This minimizes missed appointments, allowing you to deliver scheduled services and generate expected revenue.
- Focus on Patient Satisfaction: Deliver exceptional patient care from the moment they walk in. Satisfied patients are more likely to return for follow-up care and recommend your practice to others, boosting your patient base and overall revenue.
Efficient Patient Care to Enhance Cash Flow:
- Optimize Scheduling Processes: Minimize patient wait times and ensure efficient clinic flow. This allows you to see more patients throughout the day, maximizing your earning potential.
- Document Services Thoroughly: Detailed and accurate medical records are essential for proper coding and claim justification. Investing in efficient documentation practices ensures you capture all billable services.
- Utilize Technology for Streamlining Processes: From electronic health records (EHR) to online appointment scheduling, technology can streamline patient interactions and billing workflows, freeing up valuable staff time and resources.
Your Efficiency Partner
Implementing these strategies requires a comprehensive approach.
- Enhance coding accuracy and efficiency
- Automate repetitive tasks and streamline workflows
- Boost patient communication and satisfaction
- Optimize scheduling and documentation practices
Patient Verification and Account Information Management in Medical Billing
Accurate patient verification and meticulous account information management are crucial for efficient billing. Errors in patient data can lead to claim denials and delays. This post dives into actionable strategies to strengthen these areas:
- Streamlining Verification Processes
- Ensuring Accurate Account Management
These improvements empower your practice and maximize reimbursements.
Streamlining the Intricacies of Insurance Verification:
- Harnessing the Power of Electronic Verification Tools: Gone are the days of laborious phone calls and waiting on hold. Invest in cutting-edge electronic eligibility verification systems that integrate seamlessly with your billing software. These systems allow you to obtain real-time insurance coverage information for patients at the point of scheduling or upon arrival. This real-time access minimizes the risk of denied claims due to outdated or inaccurate insurance details, saving your practice time, money, and frustration.
- A Strategy for Success: Don’t wait for surprises on claim submission day. Develop a proactive verification strategy that ensures you have the most up-to-date and accurate insurance information for every patient before they receive services.
This can be achieved by:- Implementing automated pre-appointment verification workflows within your billing software.
- Training your front desk staff to request and verify insurance information during the appointment scheduling process.
- Encouraging patients to update their insurance information online through a secure patient portal (more on that later!).
- Implementing automated pre-appointment verification workflows within your billing software.
- Communication is Key: Empowering Patients and Staff: Even with the most robust verification systems, clear and concise communication remains paramount. Equip your staff with the skills to effectively communicate insurance information with patients. This includes:
- Explaining co-pays, deductibles, and any potential patient responsibility in clear and understandable language, tailored to each patient’s specific plan.
- Providing patients with written estimates of their out-of-pocket costs whenever possible.
- Training staff to answer patient questions regarding insurance coverage with confidence and empathy.
- Explaining co-pays, deductibles, and any potential patient responsibility in clear and understandable language, tailored to each patient’s specific plan.
Enhancing Accuracy in Patient Account Information Management:
- Standardization: The Bedrock of Accuracy: Develop and implement standardized data collection procedures across your entire practice. This ensures that all necessary patient demographics, insurance information, and contact details are captured consistently and accurately. Standardization can be achieved through:
- Creating standardized forms for patient intake, ensuring all required fields are clearly labeled and easy to understand.
- Developing training modules for new staff members on proper data collection procedures.
- Utilizing electronic forms and online patient portals to minimize manual data entry errors.
- Creating standardized forms for patient intake, ensuring all required fields are clearly labeled and easy to understand.
- Data Validation: A Safety Net for Success: Human error is inevitable. However, its impact on your billing processes can be mitigated by implementing robust data validation measures within your billing system. These measures can include:
- Automated data checks that identify and flag inconsistencies or missing information in patient records.
- Real-time address verification tools to ensure accurate delivery of patient statements and communications.
- Internal audits conducted periodically to identify any recurring data entry errors and implement corrective actions.
- Automated data checks that identify and flag inconsistencies or missing information in patient records.
- Patient Self-Service: Empowering Ownership:
In today’s digital age, empower your patients to take an active role in managing their healthcare information. Develop and promote a user-friendly patient self-service portal that allows patients to:- Update their demographic and insurance information in real-time.
- View their statements and download electronic copies for their records.
- Schedule appointments and make online payments for their outstanding balances.
- Update their demographic and insurance information in real-time.
Reaping the Rewards of a Fortified Foundation:
By prioritizing accurate patient verification and meticulous account information management, you unlock a multitude of benefits that empower your practice to thrive:
- Reduced Claim Denials: Accurate insurance and patient information minimizes the risk of denials due to coverage issues or missing data. This translates directly to faster claim processing, improved cash flow, and fewer administrative headaches for your staff.
- Enhanced Patient Satisfaction: Clear and accurate billing communication fosters trust and reduces patient confusion regarding their bills. When patients understand what they owe and why, they are more likely to pay their bills on time and maintain a positive relationship with your practice.
- Improved Staff Efficiency: Streamlined verification processes and accurate patient information free up valuable staff time previously spent chasing down missing information, correcting errors, and resolving billing disputes. This allows your staff to focus on what matters most – delivering exceptional patient care.
Building a Solid Foundation in Medical Billing
Understanding the complexities of medical billing and the critical role of accurate patient verification and account information management is essential for smooth operations and financial stability.
Here are key areas to focus on for building a strong foundation:
- Streamlining Verification Processes: Implement efficient procedures to verify patient demographics and insurance eligibility upfront. Consider electronic verification systems for real-time data access.
- Ensuring Accurate Account Management: Develop a system for collecting and managing patient account information meticulously. Utilize data validation tools to flag missing information and identify potential errors.
- Patient Self-Service Options: Provide a secure and user-friendly patient portal for patients to manage their account information, reducing the administrative burden on your staff.
- Staff Training: Invest in ongoing training programs to equip your team with the knowledge and skills for effective communication, data collection, and proactive verification procedures.
By focusing on these areas, you can build a solid foundation for your medical billing practices, minimizing errors, maximizing reimbursements, and achieving greater financial stability.
Investing in a Proactive Approach:
The benefits of prioritizing patient verification and account information management extend far beyond immediate cost savings. By fostering a culture of accuracy and efficiency within your practice, you create a foundation for long-term success. Reduced denials, improved cash flow, and enhanced patient satisfaction all contribute to a more sustainable and profitable practice environment.
Your Partner on the Path to Efficiency
We believe that every successful medical practice deserves a solid foundation for its billing processes. We are committed to partnering with you to streamline your verification and data management, optimize your workflows, and empower your practice to achieve its full potential.
Optimizing Charge Capture for Streamlined Medical Billing
Capturing all billable services rendered during a patient encounter is crucial for maximizing revenue and streamlining medical billing. Missed charges directly translate to lost revenue, impacting your practice’s financial health.
Utilizing Technology for Timely and Accurate Charge Capture:
The days of manual charge capture are fading. Modern technology offers a plethora of tools to streamline this process and minimize errors:
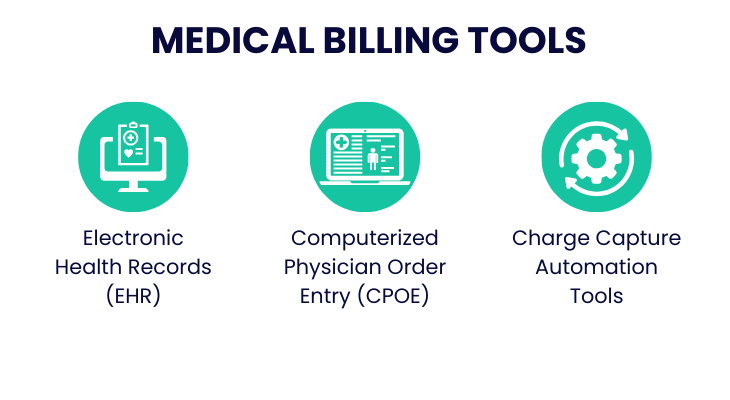
- Electronic Health Records (EHR): An integrated EHR system allows providers to seamlessly document services and link them to the appropriate codes directly within the patient’s chart. This minimizes the risk of missed charges and ensures accurate documentation for claim justification.
- Computerized Physician Order Entry (CPOE): CPOE systems allow physicians to electronically order tests, procedures, and medications. These orders automatically populate the billing system with the relevant charges, ensuring timely capture.
- Charge Capture Automation Tools: Invest in software that automates charge capture based on pre-defined rules and coding guidelines. These tools can significantly reduce the administrative burden on your staff and minimize errors.
Beyond Technology: Human Optimization Strategies:
Technology plays a crucial role, but human intervention remains necessary:
- Standardization of Documentation Practices: Develop standardized templates and workflows for documenting services. This ensures all necessary information is captured consistently and facilitates accurate coding.
- Provider Education and Training: Educate your physicians and other providers on the importance of complete and accurate documentation. Invest in training on proper coding practices to ensure they select the most appropriate codes for services rendered.
- Auditing and Feedback: Implement a system for regularly auditing charts to identify missed charges. Use this information to provide constructive feedback to providers and refine your documentation and coding processes.
Ensuring Smooth Submission of Claims to Insurance Companies:
Once charges are captured accurately, the final step is ensuring smooth claim submission to insurance companies:
- Eligibility Verification: Prior to service delivery, verify patient insurance coverage and benefits. This minimizes the risk of denials due to coverage issues.
- Claim Scrubbing: Utilize software tools to scrub claims for errors and inconsistencies before submission. This proactive approach identifies and rectifies errors that could lead to delays or denials.
- Electronic Claims Submission: Embrace electronic claim submission for faster processing and fewer errors compared to paper claims.
The Benefits of Optimized Charge Capture:
By optimizing your charge capture processes, you unlock a multitude of benefits:
- Maximized Reimbursement: Capture all billable services to ensure you receive the full reimbursement you deserve from insurance companies.
- Reduced Administrative Costs: Streamlined processes minimize time spent on manual charge capture and error correction, freeing up valuable staff resources.
- Improved Cash Flow: Faster claim processing and fewer denials lead to faster reimbursements and improved cash flow for your practice.
Optimizing Charge Capture
An efficient partnership that is a comprehensive suite of solutions to empower your practice in optimizing charge capture, including:
- Implementation and integration of EHR and CPOE systems
- Customization and configuration of charge capture automation tools
- Provider education and training programs on coding and documentation best practices
- Auditing and feedback services to identify and rectify missed charges
- Electronic claims submission and scrubbing services
Shortening the Time Between Discharge and Final Bills in Medical Billing
Timely billing is crucial in healthcare. Patients deserve clear and accurate bills soon after discharge. Here, we explore strategies to shorten the time between discharge and final bill delivery, while maintaining accuracy and efficiency:
Prompt Delivery of Final Bills to Patients:
- Streamlined Claim Submission: Implement efficient processes for claim submission to insurance companies. Utilize electronic claims submission for faster processing compared to paper claims.
- Automated Billing Processes: Leverage technology to automate repetitive tasks like charge capture, coding, and claim generation. This minimizes manual work and expedites the billing cycle.
- Clear Communication: Inform patients upfront about the estimated timeframe for receiving their final bill. This sets realistic expectations and fosters trust.
Balancing Speed with Accuracy:
While speed is important, accuracy remains paramount. Here’s how to strike the right balance:
- Prioritize Coding Accuracy: Invest in proper coder training and robust quality checks to minimize errors during the coding process. This reduces the need for rework and delays in final bill generation.
- Conduct Pre-Bill Reviews: Implement a system for pre-bill reviews before sending the final bill to the patient. This allows for catching and rectifying any errors before they reach the patient, ensuring accuracy and minimizing the risk of disputes.
- Embrace Electronic Billing: Offer patients the option to receive their bills electronically. This is not only faster but also reduces paper waste and promotes environmentally friendly practices.
Allowing Sufficient Time for Claim Reprocessing (if Required):
Even with the best efforts, denials may occasionally occur. Here’s how to handle them efficiently:
- Clear Denial Management Protocols: Develop a clear and efficient system for responding to claim denials. This should include timely communication with the insurance company, gathering necessary documentation for appeals, and resubmitting corrected claims.
- Transparency with Patients: Keep patients informed about any denials and the steps being taken to resolve them. This fosters trust and understanding.
- Consider Partial Billing: In some cases, consider issuing a partial bill for undisputed charges while the appeal process for denied charges is ongoing. This provides patients with some clarity regarding their financial obligation.
The Benefits of Timely Billing:
By shortening the time from discharge to final bill, you unlock several benefits:
- Improved Patient Satisfaction: Patients appreciate receiving their bills promptly, allowing them to budget and pay their bills on time.
- Enhanced Cash Flow: Faster billing leads to faster payments from patients, improving your practice’s cash flow.
- Reduced Administrative Burden: A streamlined billing cycle frees up valuable staff time previously spent tracking down missing information and resolving billing inquiries.
Minimizing Denials and Streamlining Accounts Receivable in Medical Billing
Two crucial factors impact revenue in medical billing: minimizing claim denials and reducing Accounts Receivable (A/R) days outstanding. Inefficient processes and inaccurate information can lead to:
- Increased Claim Denials: This results in lost revenue and additional work to appeal denials and resubmit claims.
- Extended A/R Days: Waiting longer for payments strains cash flow and creates financial burdens for your practice.
The Bedrock of Efficiency: Proper Coding and Accurate Information
Accurate coding and information form the cornerstone of efficient medical billing. Here’s why they are paramount:
- Specificity in Coding: The transition to ICD-10 coding necessitates a high level of detail. Precise coding ensures accurate claim representation, maximizing the chance of proper reimbursement from insurance companies.
- Data Integrity: Accurate patient demographic and insurance information are essential for claim adjudication. Errors in this data can lead to automatic denials, causing delays and administrative headaches.
- Documentation Practices: Clear and thorough documentation by physicians justifies the services rendered and supports the chosen codes. Incomplete or ambiguous documentation can raise red flags for insurers, inviting denials.
Proactive Strategies to Minimize Claim Denials:
By adopting a proactive approach, you can significantly reduce claim denials:
- Invest in Coder Training: Equip your coding staff with the knowledge and skills necessary for accurate ICD-10 coding. Regular training and proficiency testing ensure they stay up-to-date with the latest coding guidelines.
- Implement Pre-Billing Reviews: Before submitting claims, establish a system for internal review. This allows for identifying and rectifying any coding errors, missing information, or discrepancies that could trigger denials.
- Maintain Clear Communication with Providers: Foster open communication between coders and providers. Coders can clarify any ambiguities in documentation, while providers can gain a better understanding of coding requirements to ensure accurate capture of services.
Optimizing Processes for Faster Payment Processing and Reduced A/R Days:
Once you’ve minimized denials, focus on expediting payments:
- Electronic Claims Submission: Embrace electronic claim submission for faster processing compared to paper claims. This reduces the risk of errors due to manual data entry and streamlines communication with insurance companies.
- Eligibility Verification: Prior to service delivery, verify patient insurance coverage and benefits. Proactive verification minimizes the risk of denials due to coverage issues and ensures accurate claim submission.
- Clear Patient Billing Communication: Provide patients with clear and understandable explanations of their bills. This transparency fosters trust, reduces billing inquiries, and encourages timely payments.
- Offer Multiple Payment Options: Make it easy for patients to settle their bills by offering various payment options such as online portals, credit card processing, and installment plans. This flexibility caters to different patient preferences and promotes faster payments.
Optimizing Medical Billing Services for Your Practice
Optimizing medical billing requires careful consideration, and sometimes partnering with a medical billing service can be a strategic decision. This guide explores strategies for selecting the right partner and maximizing the efficiency of your chosen service.
Understanding Your Practice Needs:
Before embarking on your search, take a deep dive into your practice’s specific requirements. Consider factors like:
- Practice Size and Specialty: A solo practitioner likely has different needs compared to a large multi-specialty group. Billing services should be scalable to accommodate your practice’s volume and complexity.
- In-House Expertise: Do you have existing billing staff? If so, consider services that complement their expertise or handle overflow. If not, you may require a more comprehensive solution.
- Technology Integration: Ensure the chosen service seamlessly integrates with your existing Electronic Health Records (EHR) and Practice Management software.
Choosing the Right Partner: Aligning Features with Needs
Once you understand your practice’s needs, explore the offerings of potential medical billing services. Here are key features to consider:
- Coding and Billing Expertise: Look for a service with a team of experienced and certified coders who stay up-to-date on the latest coding regulations.
- Claim Submission and Follow-Up: Ensure the service offers electronic claim submission and handles claim denials and appeals efficiently.
- Reporting and Analytics: Robust reporting tools provide valuable insights into your practice’s billing performance and identify areas for improvement.
- Security and Compliance: The service must prioritize data security and ensure compliance with HIPAA regulations.
- Communication and Transparency: Choose a service with a dedicated team for clear and consistent communication regarding your billing processes.
Maximizing Efficiency: Getting the Most Out of Your Chosen Service
Once you’ve selected a medical billing service, take steps to ensure its optimal utilization:
- Clear Communication and Defined Expectations: Set clear expectations with your service provider regarding communication protocols, turnaround times, and reporting needs.
- Data Accuracy and Ongoing Training: Maintain accurate patient demographic and insurance information within your practice management system. Consider offering ongoing training to your staff on proper documentation practices to minimize errors.
- Performance Monitoring and Collaboration: Regularly review reports and performance metrics provided by your billing service. Schedule meetings to discuss areas for improvement and collaborate on optimizing workflows.
Remember, selecting the right medical billing service is an investment in your practice’s future. By carefully considering your needs, evaluating available options, and maximizing efficiency, you can ensure a seamless and profitable billing operation.
Ensuring Quality Patient Experience While Minimizing Revenue Cycle Gaps in Medical Billing
Exceptional medical billing practices go beyond just maximizing revenue. Ideally, they should seamlessly integrate with quality patient care. This fosters trust and satisfaction for your patients while ensuring financial stability for your practice. Here’s how to achieve this balance and minimize revenue cycle gaps without compromising patient experience:
Understanding the Revenue Cycle and Its Impact:
The revenue cycle encompasses all administrative and clinical functions involved in collecting payment for services rendered. Revenue cycle gaps occur when any step in this cycle experiences delays or errors. These gaps can significantly impact your practice’s bottom line.
Balancing Patient Care with Revenue Generation:
While revenue generation is essential, patient care remains the heart of healthcare. Here’s how to strike the right balance:
- Invest in Staff Training: Equip your staff with communication and interpersonal skills to ensure a positive and welcoming environment for patients.
- Prioritize Clear Communication: Communicate clearly with patients about potential out-of-pocket costs and financial assistance options upfront. This fosters trust and reduces billing surprises.
- Offer Flexible Payment Options: Provide patients with various payment options, such as online portals, credit card processing, and installment plans. This caters to different financial situations and promotes timely payments.
Strategies to Minimize Revenue Cycle Gaps:
By focusing on efficiency and accuracy, you can minimize gaps throughout the revenue cycle:
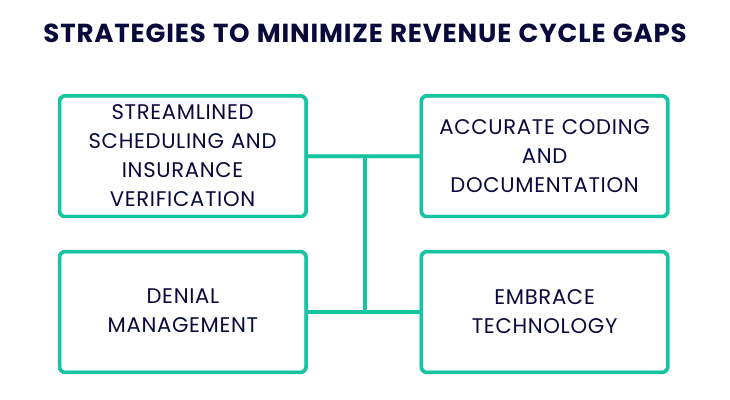
- Streamlined Scheduling and Insurance Verification: Implement efficient scheduling processes and prioritize pre-appointment insurance verification. This minimizes the risk of denied claims due to coverage issues.
- Accurate Coding and Documentation: Invest in proper coder training and robust quality checks to ensure accurate coding from the start. Clear and complete documentation by physicians further strengthens claim justification.
- Embrace Technology: Utilize electronic health records (EHR) and automated claim submission tools to streamline workflows and minimize manual errors.
- Denial Management: Develop a system for promptly addressing and resolving claim denials. This expedites the collection process and reduces outstanding receivables.
Optimizing Your Medical Billing Practices for Success
In today’s dynamic healthcare landscape, efficient and optimized medical billing practices are no longer a luxury – they are a necessity. By prioritizing accurate medical billing processes from the outset, you can streamline workflows, minimize errors, and ensure timely reimbursements. This not only translates to a healthier bottom line for your practice but also empowers you to focus on what matters most – delivering exceptional patient care.
We stand ready to be your trusted partner in this journey. We offer a comprehensive suite of solutions designed to address every aspect of your medical billing needs, from patient verification and account information management to optimizing charge capture and ensuring timely claim submission. With us by your side, you can achieve the perfect balance: maximizing revenue cycle efficiency through medical billing best practices while fostering a positive patient experience.
Don’t let inefficient medical billing processes hinder your practice’s success. Contact us today and schedule a free consultation to learn how we can help you optimize your billing operations and achieve long-term financial stability. Contact Us Today!