The medical billing process is a fundamental aspect of the healthcare industry. It serves as the bridge between healthcare services rendered and proper reimbursement for those services.
Understanding the intricacies of this process is vital for healthcare providers, administrators, and patients alike. In this section, we will delve into the explanation of the medical billing process, highlighting its significance and the importance of comprehending its complexities.
Explanation of the Medical Billing Process
The medical billing process encompasses a series of steps that healthcare providers must follow to receive payment for their services.
From patient registration to claim submission and payment collection, each stage is crucial in ensuring that healthcare providers are compensated fairly for their expertise and care.
Importance of Understanding the Process
Understanding the medical billing process is essential for healthcare professionals to navigate the complexities of reimbursement effectively. It enables providers to streamline their billing operations, reduce errors, and optimize revenue cycles.
For patients, understanding the billing process can demystify healthcare costs, empower informed decision-making, and foster transparency in financial transactions within the healthcare system.
By grasping the nuances of the medical billing process, stakeholders can enhance operational efficiency, improve financial outcomes, and ultimately contribute to a more seamless and transparent healthcare experience for all parties involved.
Understanding the Medical Billing Process
The medical billing process is a critical aspect of the healthcare industry, ensuring that healthcare providers receive proper compensation for the services they provide. This process involves a series of steps that must be meticulously followed to guarantee accurate reimbursement.
Let’s delve into an overview of the steps involved, the importance of each step, and clarify the terminology associated with the medical billing process based on the information provided in the sources.
Overview of Steps Involved

- Patient Registration: The initial step in the medical billing process involves collecting essential demographic and insurance information from the patient to establish a comprehensive patient file.
- Confirming Financial Responsibility: Determining the patient’s insurance coverage and financial obligations for the visit is crucial to understanding which services will be covered and which costs the patient will be responsible for.
- Superbill Creation: During check-in, patients provide the necessary information, and medical reports are translated into diagnosis and procedure codes to create a detailed superbill.
- Claims Generation: Medical billers use the superbill to prepare a medical claim that complies with payer and HIPAA standards before submission to the insurance company.
- Claims Submission: Once the claim is meticulously reviewed for accuracy and compliance, it is electronically transmitted to a clearinghouse or directly to high-volume payers like Medicaid.
- Monitor Claim Adjudication: Adjudication involves payers evaluating medical claims to determine their validity and the reimbursement amount, which can result in acceptance, rejection, or denial of the claim.
- Patient Statement Preparation: After claim processing, patients are billed for any outstanding charges, including a breakdown of services provided, costs, insurance coverage, and patient responsibility.
- Statement Follow-Up: The final step involves ensuring timely payment by following up with patients on outstanding bills and initiating collection procedures if necessary.
Importance of Each Step in the Process
- Patient Registration: Establishes the foundation for accurate billing by capturing essential patient information.
- Confirming Financial Responsibility: Ensures transparency in costs and responsibilities, preventing billing discrepancies.
- Superbill Creation: Facilitates accurate coding and documentation of services provided during the visit.
- Claims Generation: Critical for submitting accurate claims that comply with payer and regulatory standards.
- Claims Submission: Enables efficient communication between healthcare providers and insurers for timely reimbursement.
- Monitor Claim Adjudication: This ensures that claims are processed accurately and providers receive fair reimbursement.
- Patient Statement Preparation: Provides patients with a clear breakdown of charges, promoting transparency in billing practices.
- Statement Follow-Up: Essential for managing accounts receivable and ensuring timely payment for services rendered.
Clarification of Terminology
In medical billing, a comprehensive understanding of key terminology is essential for healthcare providers to navigate the complexities of billing and reimbursement effectively.
Let’s expand on clarifying important terms based on the information provided in the sources, incorporating additional terminologies to enrich our understanding.
- Claim: A claim is a formal request for payment submitted by healthcare providers to insurance companies for services rendered. It outlines the services provided, their associated costs, and the reimbursement sought from the insurance payer.
- Adjudication: Adjudication is the process by which insurance payers evaluate and determine the validity and reimbursement amount of medical claims. It involves thoroughly reviewing submitted claims to ensure compliance with regulations and policies.
- Coding: Coding involves assigning specific codes to medical procedures and diagnoses for billing and reimbursement purposes. Accurate coding is crucial for documenting services accurately and facilitating communication between healthcare providers and insurance payers.
Additional Terminology:
- Allowed Amount: The amount insurance companies will pay or reimburse for a specific service or procedure.
- Aging: When an insurance claim or patient bill passes a certain period without being paid.
- Ancillary Services: Additional services a patient receives in a hospital, such as diagnostic tests, prosthetics, and physical therapy.
- Appeal: The process by which a patient objects to a denial of service by a health insurance plan.
- Applied to Deductible (ATD): Services that fall under a patient’s deductible, requiring the patient to pay before insurance coverage kicks in.
- Accounts Receivable (AR): The amount owed to a healthcare provider for services rendered but still needs to be paid.
- Bundling: Listing two or more healthcare services under one billing code.
- Claim Adjustment Reason Codes (CARCs): Codes explain why a payment was adjusted and a claim was paid differently.
- Clearinghouse: An intermediary transmitting secure electronic medical claims and financial information between providers and payers.
- Coordination of Benefits: When a patient is covered by more than one insurance plan, determine the primary and secondary coverage.
Step-by-Step Breakdown of the Medical Billing Process
- Patient Registration: The medical billing process begins with registering a new patient or updating an existing patient’s information. This step involves collecting essential demographic data, insurance details, and the reason for the patient’s visit.
- Confirming Financial Responsibility: After the patient’s registration, the healthcare provider must confirm the patient’s financial responsibility. This includes verifying the patient’s insurance coverage, deductibles, copayments, and any other financial obligations they may have.
- Patient Check-in and Check-out: When the patient arrives for their appointment, the healthcare provider must accurately document the patient’s check-in and check-out times, and any services or treatments provided during the visit. This information is then translated into a “superbill” that includes diagnosis and procedure codes.
- Preparing Claims and Checking Compliance: The medical biller uses the superbill to prepare the medical claim, ensuring that it includes accurate and compliant information, such as the appropriate diagnostic and procedure codes, as well as any necessary supporting documentation.
- Transmitting Claims: Once the claim has been prepared and checked for accuracy, it is transmitted to the appropriate insurance payer, either electronically or through traditional paper-based methods.
- Monitoring Adjudication: After the claim has been submitted, the healthcare provider must monitor the adjudication process, which involves the insurance reviewing and determining the claim’s validity and the appropriate reimbursement amount.
- Generating Patient Statements: If the insurance payer’s reimbursement does not cover the full cost of the services provided, the healthcare provider must generate a patient statement outlining the remaining balance and any payment options available to the patient.
- Following up on Patient Payments and Handling Collections: Finally, the healthcare provider must follow up on patient payments and handle any necessary collections processes, ensuring that they receive the full reimbursement for the services they have provided.
By understanding and implementing this comprehensive step-by-step medical billing process, healthcare providers can streamline their operations, improve revenue cycle management, and ensure timely and accurate reimbursement for their services.
Importance of Accuracy and Compliance in Medical Billing
Accuracy and compliance are foundational pillars of the medical billing process, essential for the financial health of healthcare providers, patient trust, and overall operational efficiency.
Let’s delve into a detailed exploration of the importance of accuracy and compliance in medical billing based on the insights from the provided sources.
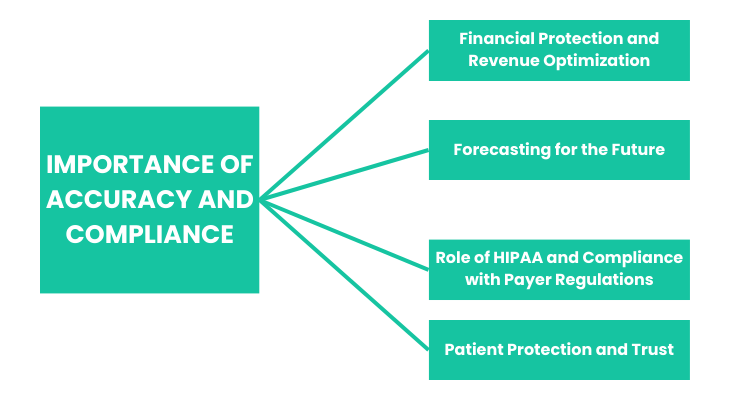
Financial Protection and Revenue Optimization
Accurate billing practices are paramount for healthcare providers enabling precise revenue forecasting, cost analysis, and informed decision-making.
By maintaining accuracy in billing and coding, healthcare practices can analyze revenue data effectively, identify cost structures, and make informed decisions regarding staffing, patient outreach, and service line expansions.
Accurate billing not only safeguards the financial stability of the practice but also ensures that the practice receives the full reimbursement it is entitled to, preventing financial losses and potential legal liabilities.
Patient Protection and Trust
Accurate medical coding and billing directly impact patient care and experience by preventing financial burdens and delays associated with billing inaccuracies.
Patients rely on accurate billing information to understand their healthcare costs, make informed decisions, and trust the transparency of their healthcare providers. Inaccurate billing can harm patient trust, compromise the quality of care, and lead to financial burdens for patients.
By prioritizing accuracy and compliance, healthcare providers can protect patient interests, enhance patient-provider relationships, and foster a culture of trust and transparency in healthcare delivery.
Forecasting for the Future
Compliance with medical coding protocols and accurate billing practices enable healthcare providers to forecast the future effectively.
When billing practices are compliant and accurate, healthcare practices can ensure precise billing to patients and insurance companies, facilitating revenue forecasting and financial planning.
Accurate billing practices empower healthcare providers to make informed decisions, optimize revenue cycles, and prepare for future financial challenges effectively.
Role of HIPAA and Compliance with Payer Regulations
The role of the Health Insurance Portability and Accountability Act (HIPAA) in medical billing is pivotal. It establishes standards for protecting patient health information and ensuring ethical operations within healthcare organizations.
Compliance with HIPAA regulations is mandatory to maintain patient confidentiality, data security, and legal compliance. Additionally, adherence to payer regulations is essential to ensure timely and accurate reimbursement, minimize claim denials, and maintain operational efficiency within healthcare practices.
By emphasizing accuracy and compliance in medical billing practices, healthcare providers can optimize revenue generation, enhance patient satisfaction, maintain regulatory compliance, and fortify their financial foundations in the dynamic landscape of healthcare delivery.
Benefits of Electronic Claims Submission
Electronic claims submission offers a streamlined and efficient process for healthcare providers to submit patient claims to payers. Let’s delve into the benefits of electronic claims submission based on the insights from the provided sources:
Efficiency and Speed of Electronic Submission
- Time and Resource Savings: Electronic claims submission eliminates the need for paper claims, reducing the time and resources required for claims submission. It simplifies record-keeping, streamlines operations, and frees administrative time for other essential tasks.
- Pre-Audit for Errors: Electronic submission allows pre-auditing claim fields to identify potential errors before submitting to payors. This proactive approach ensures accuracy and completeness, reducing the likelihood of lost or incomplete claims.
- Instantaneous Submission: Claims can be sent in bulk easily with almost instantaneous submission, reducing the need for manual processing and minimizing the number of staff required for claim submission.
Reduction of Errors and Administrative Costs
- Faster Processing and Payment: Electronic claims are processed faster than paper claims, leading to quicker payment turnaround times. Claims are given priority and processed within days, enhancing cash flow for healthcare providers.
- Error Detection: Electronic claims submission allows for earlier detection of errors, reducing the likelihood of claims being rejected or denied payment. Claims are edited before submission, ensuring accuracy and completeness.
- Lower Administrative Costs: Electronic claims submission reduces administrative, postage, and handling costs associated with paper claims. It increases efficiency, reduces paperwork-related expenses, and enhances overall cost-effectiveness.
Comparison with Manual Claims Processing
- Efficiency and Cost-Effectiveness: Electronic claims submission offers a straightforward, efficient, and cost-effective process compared to manual claims processing. It reduces the administrative burden and expense of manual claims submission, resulting in significant financial savings for healthcare providers and payers.
- Time Savings: Electronic claims processing is faster and more efficient than manual processing, leading to quicker reimbursement rates and improved accounts receivable management. The average cost of processing electronic claims is lower than processing paper claims, enhancing operational efficiency and reducing payment delays.
Based on the information provided in the search results, here are the key challenges and solutions in the medical billing process:
Common Challenges Faced in the Process:
- Coding Errors: Inaccurate or incomplete coding can lead to claim denials and payment delays. Solutions include improving communication between clinicians and billing staff, providing regular training on coding requirements, and leveraging technology like computer-assisted coding.
- Increasing Claim Denials: Denials can result from evolving regulations, changing payer policies, and inadequate documentation. Strategies include implementing robust pre-authorization processes, enhancing documentation practices, and staying up-to-date with billing regulations.
- Multiple Claims Submission: The high volume of claims and diverse payer requirements can lead to errors and rejected/delayed submissions. Solutions involve using claims management systems, thorough staff training, and regular audits to identify and fix errors.
- Lack of Skilled Billing Professionals: The complexity of medical coding, documentation, and regulations requires specialized expertise. Addressing this challenge requires investment in training and education programs for billing staff.
- Inaccurate Patient Details: Errors in patient information, such as misspelled names or outdated insurance details, can cause claim denials and delays. Emphasizing accuracy during the patient registration process is crucial.
- Poor Denial Management Process: Ineffective denial tracking, analysis, and resolution can lead to revenue leakage. Implementing robust denial management systems, staff training, and clear communication with payers are key solutions.
Strategies for Overcoming Billing Obstacles:
- Leveraging Technology: Adopting medical billing software, computer-assisted coding, and electronic claims submission can improve efficiency, reduce errors, and streamline the overall billing process.
- Enhancing Documentation and Compliance: Mitigating billing challenges requires maintaining thorough documentation, staying up-to-date with coding guidelines, and ensuring compliance with HIPAA and payer regulations.
- Investing in Staff Training and Education: Providing regular training and education for billing professionals on coding, documentation, and evolving regulations can help address the shortage of skilled personnel and improve overall billing accuracy.
Importance of Staying Updated with Industry Changes:
The medical billing landscape is constantly evolving, with changes in regulations, coding systems, and payer policies.
Healthcare providers must stay vigilant and proactive in monitoring industry updates to adapt their billing practices accordingly. Failure to keep up with these changes can lead to significant financial and compliance risks.
By addressing these common challenges and implementing effective strategies, healthcare providers can optimize their medical billing processes, enhance revenue cycle management, and ensure the financial stability of their healthcare organizations.
Summing Up
The medical billing process is a complex and multifaceted aspect of the healthcare industry, but understanding its intricacies is crucial for healthcare providers to ensure timely and accurate reimbursement.
This comprehensive guide has explored the various steps involved in the medical billing process, the importance of accuracy and compliance, the benefits of electronic claim submission, and the common challenges and solutions in medical billing.
Throughout this guide, we have emphasized the significance of each step in the medical billing process, from patient registration to claim submission and payment collection.
We have also highlighted the critical role of HIPAA compliance, coding accuracy, and adherence to payer regulations in ensuring the financial stability and operational efficiency of healthcare providers.
The transition to electronic claim submission has brought numerous benefits, including improved efficiency, reduced errors, and lower administrative costs.
By leveraging technology and adopting best practices, healthcare providers can streamline their medical billing processes and focus on delivering high-quality patient care.
However, the medical billing landscape has its challenges. Healthcare providers must proactively address issues such as claim denials, patient non-payment, and changes in payer regulations.
By staying up-to-date with industry changes and implementing effective strategies, healthcare providers can overcome these obstacles and ensure the long-term success of their medical billing operations.
By embracing best practices, leveraging technology, and staying adaptable to change, healthcare providers can enhance the overall efficiency and effectiveness of their medical billing processes, ultimately benefiting both their organizations and the patients they serve.
Contact Promantra for Your Medical Billing Needs
If you’re a healthcare service provider looking for a medical billing partner, you’re in the right place. We at Promantra have more than two decades of experience with medical billing and RCM.
Let us streamline your billing and collections process, reducing revenue leakage, minimizing claim denials, and accelerating claim processing. Experience improved cash flow and increased revenue.
Our tailored RCM services are designed to meet HIPAA and CMS standards, aligning with your unique organizational needs. By outsourcing administrative tasks and refining processes, we help healthcare organizations cut costs associated with the revenue cycle.
Our experienced professionals ensure you stay ahead of the latest trends and technological solutions, maximizing operational efficiency. Trust Promantra to elevate your revenue cycle management.
Get in touch with our team today to learn more about our medical billing services.