In the ever-evolving US healthcare industry, providers must stay on top of medical billing trends. A recent American Medical Association (AMA) study found that nearly 25% of physician practices experience billing errors, leading to significant revenue loss. Efficient and accurate billing practices ensure timely reimbursements and contribute to your practice’s financial health.
Here, we’ll delve into the top medical billing trends shaping 2024, equipping you with the knowledge to navigate the complexities of healthcare reimbursement and optimize your revenue cycle.
This year, we continue emphasizing technology and automation to streamline processes, improve accuracy, and enhance patient experiences. Regulatory changes and an increased focus on data security are also crucial factors impacting medical billing in 2024. Let’s explore these trends in more detail and explore how to leverage them to strengthen your practice’s financial footing.
This statistic from American Medical Association (AMA) highlights the prevalence of billing errors and their financial impact, emphasizing the importance of staying informed about medical billing trends.
Top Medical Billing Trends for US Healthcare Providers in 2024
Let’s dive into the blog’s heart and explore the top medical billing trends for US healthcare providers in 2024. Here are some key areas to consider:
Technological Advancements:
- Automation and Artificial Intelligence (AI): We’ll see a continued rise in automation for tasks like coding, claims scrubbing, and prior authorization. AI can further enhance automation by analyzing data to identify errors and optimize workflows.
- Telehealth Billing Integration: As telehealth services become more prevalent, seamless integration between telehealth platforms and billing systems will ensure efficient and accurate billing for virtual consultations.
Focus on Patient Engagement and Revenue Cycle Management:
- Patient-Centric Billing: Practices must prioritize clear and transparent communication with patients about their billing responsibilities. This includes providing easy-to-understand explanations of charges and offering flexible payment options.
- Emphasis on Revenue Cycle Management (RCM): A data-driven approach to RCM will be vital in identifying areas for improvement and optimizing the entire revenue cycle, from patient scheduling to claim reimbursement.
Regulatory Changes and Data Security:
- ICD-11 Implementation: The planned implementation of ICD-11 (International Classification of Diseases, 11th Revision) will necessitate updates to coding practices and billing systems. Staying informed about the transition timeline and requirements is crucial.
- Heightened Cybersecurity Concerns: With the ever-growing threat of cyberattacks, healthcare providers must prioritize robust data security measures to protect sensitive patient information.
These are just some of the top medical billing trends shaping the US healthcare landscape 2024. In the following sections, we’ll delve deeper into each trend, exploring its implications and offering actionable insights for healthcare providers to adapt and thrive in the evolving environment.
Automation and Artificial Intelligence (AI) Integration in Medical Billing
The healthcare industry is witnessing a surge in automation and AI integration within medical billing. Automation refers to using technology to streamline repetitive tasks, minimizing human intervention. Conversely, AI leverages machine learning algorithms to analyze data, identify patterns, and even make intelligent decisions.
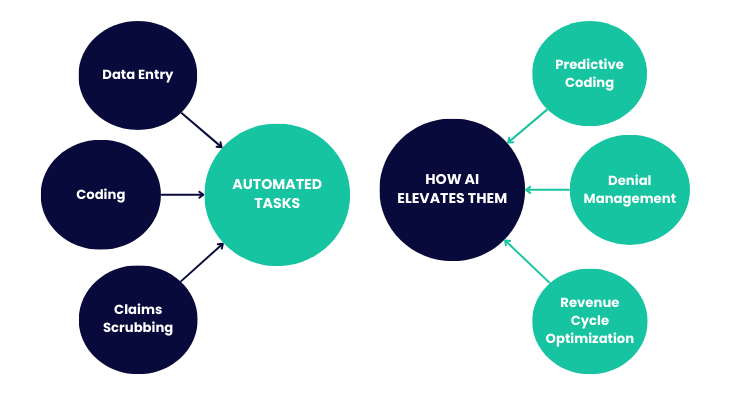
Automation in Medical Billing:
- Data Entry: Automatically populating patient information, demographics, and insurance details from Electronic Health Records (EHR) eliminates manual entry errors.
- Coding: Automation assists with assigning accurate medical codes based on diagnoses and procedures, reducing the risk of human error and improving coding efficiency.
- Claims Scrubbing: Automated tools can identify inconsistencies or missing information in claims before submission, preventing rejections and reimbursement delays.
AI in Medical Billing:
- Predictive Coding: AI can analyze historical data and suggest the most appropriate codes for specific procedures and diagnoses, further enhancing coding accuracy.
- Denial Management: AI can identify patterns in denied claims and recommend corrective actions to reduce future denials.
- Revenue Cycle Optimization: AI can analyze billing data to identify areas for improvement in the revenue cycle, leading to faster reimbursements and improved cash flow.
Benefits of Automation and AI Integration
Integrating automation and AI in medical billing offers numerous benefits:
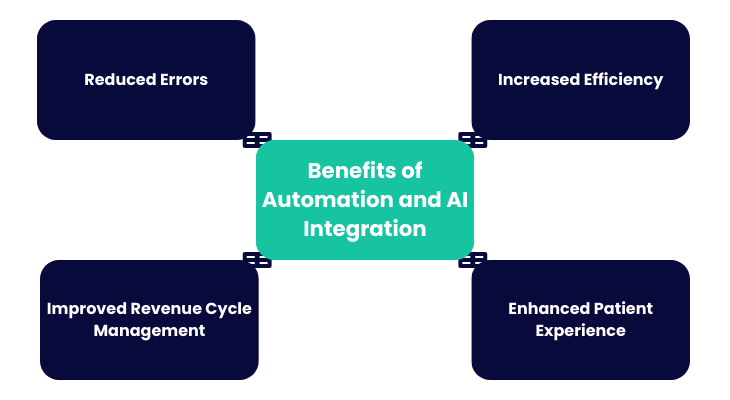
- Increased Efficiency: Automating repetitive tasks frees staff time for more complex tasks, improving overall productivity.
- Reduced Errors: Automation and AI minimize human error in data entry, coding, and claims submission, leading to cleaner claims and faster reimbursements.
- Improved Revenue Cycle Management: AI-powered insights help identify bottlenecks and optimize the entire revenue cycle, leading to faster cash flow.
- Enhanced Patient Experience: Automation can streamline patient billing inquiries and provide more transparent and timely information about their charges.
Examples of Automation and AI in Coding, Claims Processing, and Revenue Cycle Management
Here are some specific examples of how automation and AI are transforming medical billing:
- Automated coding software can analyze physician notes and suggest relevant codes, reducing coding time and improving accuracy.
- AI-powered claims scrubbing tools can automatically identify errors or missing information in claims before submission, preventing rejections and delays.
- Predictive analytics can analyze historical data to identify patients at high risk of payment delinquency, allowing providers to implement proactive collection strategies.
Impact on Efficiency and Error Reduction
Automation and AI significantly impact efficiency and error reduction in medical billing. By automating repetitive tasks and leveraging AI for data analysis, healthcare providers can:
- Reduce coding time by up to 50%.
- Decrease claim denials by 20% or more.
- Improve cash flow by accelerating reimbursements.
These improvements translate to significant cost savings and allow medical practices to focus on delivering high-quality patient care.
Value-Based Care Reimbursement Models: Adapting to a New Era of Healthcare Billing
The healthcare reimbursement landscape is shifting towards value-based care (VBC) models. This section will explore the implications of VBC for medical billing and equip you with strategies to adapt and thrive in this evolving environment.
Overview of Value-Based Care and Its Impact on Medical Billing
Traditional fee-for-service (FFS) models reimburse providers based on service volume. VBC, on the other hand, focuses on rewarding providers for the quality of care they deliver and the health outcomes achieved for patients. This shift necessitates transitioning from volume-driven billing to a more holistic approach emphasizing preventive care, chronic disease management, and patient engagement.
Shift Towards Rewarding Providers Based on Patient Outcomes
VBC models incentivize providers to:
- Focus on preventive care to keep patients healthy and reduce the need for costly interventions.
- Manage chronic conditions effectively to improve patient outcomes and reduce overall healthcare costs.
- Prioritizing patient engagement and communication empowers patients to manage their health.
Strategies for Adapting to Value-Based Care Reimbursement Models
To adapt to VBC successfully, medical practices should consider the following strategies:
- Invest in Data Analytics: Robust data collection and analysis are crucial for tracking patient outcomes and demonstrating the value of care delivered.
- Coding for Quality Measures: Accurate coding of quality measures, such as preventive care services and chronic disease management activities, is essential to maximize reimbursement under VBC models.
- Patient Engagement Strategies: Develop proactive strategies to engage patients in their care plans, encouraging preventive care and medication adherence. This can lead to improved health outcomes and reduced healthcare utilization.
Importance of Accurate Documentation and Patient Engagement
Accurate and detailed documentation of patient encounters becomes paramount in VBC models. Clear documentation ensures proper coding of quality measures and reflects the complexity of care provided.
Patient engagement is another critical element. By empowering patients to actively participate in their health, VBC models can lead to more efficient care delivery and improved overall health outcomes.
Telehealth Billing Optimization: Navigating the New Frontier
Telehealth services have become a mainstay in the healthcare industry, offering patients convenient access to care and providers a way to expand their reach. However, telehealth billing presents unique challenges and complexities. This section will equip you with strategies to optimize your telehealth billing processes, ensuring compliance and maximizing revenue capture in 2024.
Importance of Telehealth Billing in 2024
The demand for telehealth services will continue its upward trajectory in 2024. With this growth comes the need for efficient and accurate telehealth billing practices. Proper billing ensures timely reimbursements for telehealth services, allowing providers to continue offering these valuable services to patients.
Challenges and Complexities in Telehealth Billing
Telehealth billing comes with its own set of challenges:
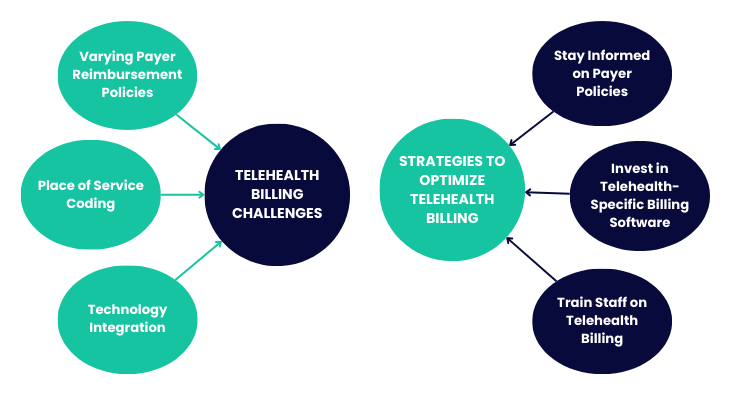
- Varying Payer Reimbursement Policies: Payers may have different policies and regulations regarding telehealth services, requiring careful verification of patient coverage and specific coding requirements.
- Place of Service Coding: Accurate coding of the place of service (POS) for telehealth encounters is crucial to avoid denials.
- Technology Integration: Seamless integration between telehealth platforms and billing systems ensures efficient claims processing and minimizes errors.
Strategies for Optimizing Telehealth Billing Processes
Here are some critical strategies for optimizing your telehealth billing processes:
- Stay Informed on Payer Policies: Regularly review and update your understanding of payer policies regarding telehealth services, including covered services, prior authorization requirements, and specific coding guidelines.
- Invest in Telehealth-Specific Billing Software: Consider implementing telehealth-specific billing software to handle the unique complexities of submission of telehealth claims.
- Train Staff on Telehealth Billing: Ensure your billing staff possesses the necessary knowledge and skills to code and submit telehealth claims accurately.
Ensuring Compliance and Maximizing Revenue Capture
By implementing these strategies, healthcare providers can navigate the complexities of telehealth billing and ensure compliance with payer regulations. This translates to maximizing revenue capture for telehealth services, allowing your practice to thrive in the evolving healthcare landscape.
Interoperability and Data Exchange: Streamlining Billing in a Connected Healthcare Ecosystem
The ability of healthcare systems, payers, and providers to seamlessly exchange data is crucial for efficient medical billing. This section will delve into the significance of interoperability, explore advancements in data exchange, and highlight the benefits of streamlining billing workflows and reducing administrative burdens.
Significance of Interoperability in Medical Billing
Interoperability ensures a smooth and secure exchange of patient data between different healthcare entities. This includes electronic health records (EHRs), billing systems, and payer platforms. Seamless data exchange eliminates the need for manual data entry, reducing errors and streamlining the entire billing process.
Advancements in Data Exchange Between Healthcare Systems, Payers, and Providers
Several advancements are paving the way for improved data exchange:
- Standardized Data Formats: Adopting standardized data formats like HL7 (Health Level Seven) facilitates smoother data exchange between disparate healthcare systems.
- Application Programming Interfaces (APIs): APIs allow different healthcare applications to communicate and share data securely, enabling real-time exchange of patient information relevant to billing.
- Health Information Exchanges (HIEs): HIEs act as secure repositories for patient data, allowing authorized providers and payers to access relevant information for billing purposes.
Impact on Billing Workflows and Administrative Burden
Enhanced interoperability significantly impacts medical billing workflows and administrative burdens:
- Reduced Manual Data Entry: Automatic data transfer between systems eliminates the need for manual data entry, minimizing errors and freeing up staff time for more complex tasks.
- Improved Claim Accuracy: Accurate and complete data transfer leads to cleaner claims with fewer denials and reimbursement delays.
- Streamlined Workflow: Automated data exchange streamlines the entire billing process, improving efficiency and reducing administrative costs.
Benefits of Enhanced Interoperability and EHR Systems
The benefits of enhanced interoperability extend beyond streamlined billing:
- Improved Patient Care: Real-time access to complete patient data allows providers to make more informed care decisions, leading to better patient outcomes.
- Reduced Costs: Reduced administrative burden and fewer claim denials translate to significant cost savings for healthcare providers.
- Enhanced Patient Engagement: Patients can access their billing information more efficiently, promoting transparency and fostering trust.
By leveraging data exchange and interoperability advancements, healthcare providers can create a more connected healthcare ecosystem, leading to a more efficient and patient-centered experience.
Patient Financial Responsibility Management: Prioritizing Transparency and Building Trust
With rising deductibles and copays, patients are increasingly responsible for a larger share of healthcare costs. This section will focus on patient financial responsibility management, equipping you with strategies to navigate this evolving landscape and build trust with your patients.
Growing Importance of Patient Financial Responsibility
The financial burden on patients is on the rise. Understanding this shift is crucial for healthcare providers. Patients are no longer passive recipients of care; they are active consumers who are mindful of costs and expect transparency.
Strategies for Effective Patient Financial Responsibility Management
Here are some key strategies for effective patient financial responsibility management:
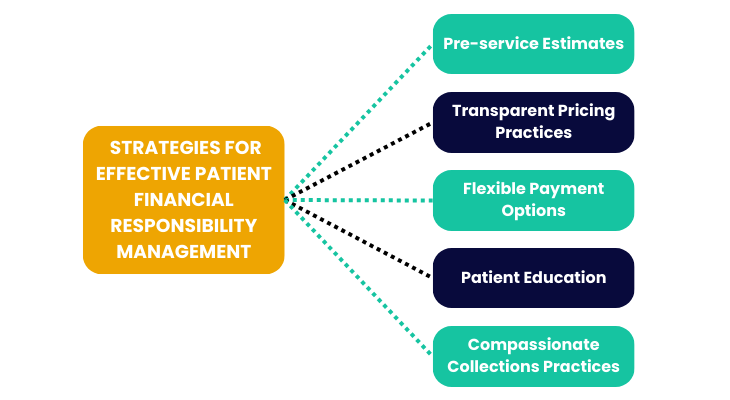
- Pre-service Estimates: Before any service is rendered, provide patients with precise and accurate estimates of their out-of-pocket costs. This text allows patients to make informed decisions about their care.
- Transparent Pricing Practices: Develop a pricing structure that is easy for patients to understand and readily available on your website and in your practice.
- Flexible Payment Options: Offer various payment options, such as online portals, installment plans, and credit card processing, to cater to different financial needs.
- Patient Education: Educate patients about their insurance coverage and explain billing processes clearly and concisely.
- Compassionate Collections Practices: Develop an empathetic approach to collections, offering financial aid options and understanding patients’ challenges.
Implementing Transparent Pricing Practices and Flexible Payment Options
Transparency in pricing builds trust with patients. Precise estimates and flexible payment plans demonstrate your commitment to patient-centered care. This can lead to improved patient experience and satisfaction along with a more positive overall patient experience.
Leveraging Patient Engagement Tools
Technology can play a crucial role in managing patient financial responsibility. Utilize online patient portals that allow patients to:
- View their billing statements electronically.
- Make secure online payments.
- Set up payment plans.
- Access cost estimates for potential services.
Patients can actively manage their healthcare finances by utilizing patient engagement tools.
Regulatory Compliance and Risk Mitigation: Navigating the Evolving Landscape
Ensuring compliance with ever-changing healthcare regulations is a cornerstone of responsible medical billing practices. This section will delve into the importance of regulatory compliance, highlight vital regulations, and offer strategies for proactive risk mitigation.
Overview of Regulatory Compliance in Medical Billing
Healthcare providers are subject to a complex set of regulations that govern their medical billing practices. Compliance with these regulations protects patient privacy, ensures accurate billing, and minimizes the risk of fraud and abuse. Here are some of the key regulations that impact medical billing:
- HIPAA (Health Insurance Portability and Accountability Act) safeguards patients’ protected health information (PHI). Medical billing practices must adhere to HIPAA regulations regarding data security and privacy.
- ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification): ICD-10-CM provides standardized codes for diagnoses and procedures used in medical billing. Accurate coding ensures proper reimbursement and compliance with payer regulations.
- CMS (Centers for Medicare & Medicaid Services) Guidelines: CMS establishes billing guidelines and rules for Medicare and Medicaid programs. Staying updated on these guidelines is crucial for providers who participate in these programs.
Importance of Proactive Monitoring and Ongoing Staff Training
A proactive approach to regulatory compliance is very crucial. Here are some key strategies:
- Regular Audits: Conduct internal audits to evaluate and address any potential billing compliance issues.
- Stay Informed of Regulatory Changes: Monitor regulatory updates from agencies like HIPAA, ICD-10-CM, and CMS regularly to ensure your billing practices remain compliant.
- Ongoing Staff Training: Implement ongoing training programs to ensure your billing staff possesses the knowledge and skill sets necessary to navigate the complexities of medical billing regulations.
Mitigating Billing-Related Risks
By prioritizing regulatory compliance, healthcare providers can mitigate various billing-related risks:
- Reduced Risk of Audits and Penalties: Compliance minimizes the risk of costly audits and potential penalties from regulatory agencies.
- Improved Reimbursement Rates: Accurate and compliant billing practices lead to fewer claim denials and faster reimbursements.
- Enhanced Patient Trust: Demonstrating a commitment to compliance builds trust with patients and strengthens your reputation.
Data Analytics for Revenue Optimization: Leveraging Data for Financial Success
In the ever-competitive world of healthcare, maximizing revenue and optimizing the billing process is crucial for a practice’s financial health. This section explores the role of data analytics in medical billing and how it empowers providers to make data-driven decisions for revenue optimization.
Role of Data Analytics in Medical Billing
Data analytics goes beyond simply collecting billing data. It involves evaluating vast amounts of information to identify trends, patterns, and areas for improvement. By utilizing data analytics tools and techniques, healthcare providers can gain valuable insights and evaluations to improve patient care, operational efficiency, and decision-making.:
- Identify Coding Inconsistencies: Analyze coding practices to detect inconsistencies and ensure accurate coding for optimal reimbursement.
- Predict Claim Denials: Utilize data to predict potential claim denials based on historical trends and payer-specific rules. This allows for proactive intervention and reduces denials.
- Optimize Denial Management: Review rejected insurance claims to determine the underlying reasons and develop plans to avoid future rejections.
- Track Revenue Cycle Performance: Gain insights into key metrics like collection rates, days in accounts receivable (AR), and write-offs to identify areas for improvement in the revenue cycle.
Utilizing Data Analytics Tools and Predictive Analytics Algorithms
Advanced data analytics tools and algorithms play a vital role in medical billing:
- Business Intelligence (BI) Tools: BI tools provide user-friendly dashboards and reports, allowing providers to visualize key billing metrics and identify trends quickly.
- Predictive Analytics: Machine learning (ML) algorithms can evaluate historical data to predict future trends, such as patient payment behavior or potential denials. This enables proactive approaches to revenue collection and claim management.
Identifying Revenue Opportunities and Optimizing Billing Processes
Data analytics empowers providers to identify untapped revenue opportunities:
- Unbilled Services: Analyze data to identify services rendered that may need to have been billed correctly or entirely.
- Patient Self-Pay Opportunities: Data can help identify patients with high deductibles or out-of-pocket costs, allowing you to offer flexible payment options to improve collections.
- Under-coded Procedures: Utilize data to detect instances where procedures may have been under-coded, leading to missed revenue opportunities.
Enhancing Financial Performance through Data-Driven Strategies
By leveraging data analytics, healthcare providers can make informed decisions to optimize billing processes and improve financial performance:
- Improved Cash Flow: Proactive denial and efficient revenue cycle management lead to faster reimbursements and improved cash flow.
- Reduced Operational Costs: Data-driven insights can help identify areas for streamlining billing processes and reducing administrative costs.
- Informed Resource Allocation: Data can guide resource allocation decisions, ensuring staff and resources are directed towards areas with the highest potential return.
Stay Ahead of Future Medical Billing Trends With Promantra
The healthcare landscape is constantly growing, and medical billing practices must adapt. Here at ProMantra, we understand the challenges and opportunities ahead in 2024.
This blog has explored some of the critical trends shaping medical billing, including:
- The Rise of Automation and AI: We are dedicated to staying at the forefront of technology advancements and excellence, offering solutions that automate repetitive tasks, improve coding accuracy, and streamline workflows.
- Focus on Value-Based Care: ProMantra is dedicated to helping providers succeed in value-based care models by providing tools and expertise to ensure accurate coding for quality measures and optimize patient engagement.
- Telehealth Billing Optimization: As telehealth services continue to grow, ProMantra offers solutions designed to handle the complexities of submission of telehealth claims and ensure proper reimbursement.
- Enhanced Interoperability and Data Exchange: We are passionate about fostering a more connected healthcare ecosystem through robust data exchange solutions that streamline billing processes and reduce administrative burdens.
- Patient Financial Responsibility Management: ProMantra recognizes the importance of patient-centered care. We provide tools and resources to help providers build patient trust through transparent pricing, flexible payment options, and clear communication.
- Regulatory Compliance and Risk Mitigation: Our team of experienced experts stays current on the latest regulations and provides ongoing support to ensure your billing practices remain compliant and minimize risks.
- Data Analytics for Revenue Optimization: ProMantra leverages cutting-edge data analytics tools to empower you with actionable insights for optimizing your revenue cycle, identifying untapped revenue opportunities, and making data-driven decisions for long-term financial success.
At ProMantra, we are dedicated to partnering with healthcare providers to navigate the ever-changing medical billing landscape. We provide a broad suite of solutions and ongoing support to ensure your practice thrives in 2024 and beyond. By embracing these trends and partnering with ProMantra, you can optimize your billing processes and maximize reimbursements.
Contact us today to learn more about how ProMantra can help your practice adapt to the evolving world of medical billing.




