One of the core functions of any healthcare organization is medical billing. This is the process of submitting claims to insurance companies to get the reimbursement due for services provided.
Medical billing can be a painstaking process, even though advancements like EHRs (Electronic Health Records), have made the process a lot more streamlined. A lot of healthcare organizations now find it more beneficial to outsource the medical billing process rather than handling it in-house.
Why is handling this process in-house difficult? What are the benefits of outsourcing medical billing? To answer these questions and more, here’s everything you need to know about outsourcing medical billing.
Challenges of In-House Medical Billing
To understand why a lot of healthcare organizations prefer outsourcing medical billing, let’s first delve into the challenges of handle the function in-house.
Staffing and Training Costs
Staffing and training are major cost for healthcare organizations. Not only do a lot of them operate without the assistance of staffing organizations, but they also need to constantly upskill their existing staff to keep up with changing technologies and regulations.
The training required to handle medical billing in-house, considering it requires knowledge of codes, regulations and attention to detail to ensure claims are not denied and revenue goals in billing operations are met, will only add to these costs.
Healthcare Regulations and Policies
Healthcare providers need to stay abreast of changing policies and regulations like HIPAA. This ensures data security, accurate billing, and safeguards revenue.
To streamline internal workflows and function efficiently, healthcare providers must integrate these policies and regulations into their billing operations, which can make the process painstaking.
Time and Effort
Medical billing is a tedious and time consuming process. As a result, revenue performance and operational efficiency is often compromised.
The tedious nature of the process often also leads to errors in billing and delayed payments, not to mention the increased costs due to the hours of manual labor involved.
Benefits of Outsourcing Medical Billing
Let’s now make our case in favor of outsourcing medical billing even stronger by taking a look at some compelling benefits.
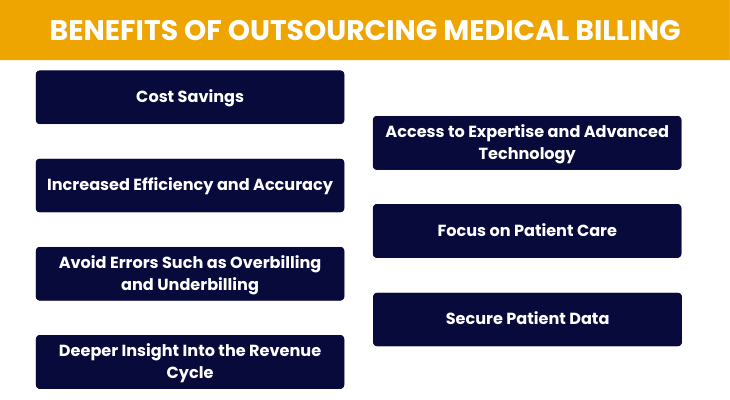
Cost Savings
Outsourcing medical billing allows healthcare providers to eliminate the need for maintaining an in-house billing department, thereby reducing staffing costs related to salaries, benefits, and training programs.
Additionally, outsourcing eliminates the need to invest in expensive billing software and infrastructure, resulting in significant overhead cost savings for the organization.
Access to Expertise and Advanced Technology
Billing companies employ skilled professionals who are well-versed in medical coding, billing regulations, and industry best practices. These experts leverage advanced billing software and technology solutions to automate processes, minimize errors, and ensure compliance with complex healthcare regulations such as HIPAA.
By tapping into this specialized expertise and technology, healthcare providers can streamline their billing operations and achieve higher levels of accuracy and efficiency.
Increased Efficiency and Accuracy
Outsourcing billing tasks to experienced professionals allows healthcare providers to streamline their revenue cycle management processes. These professionals have the knowledge and resources to efficiently handle tasks such as claim submission, payment posting, and denial management.
As a result, healthcare organizations experience faster reimbursements, reduced claim denials, and improved cash flow, ultimately enhancing overall operational efficiency and financial performance.
Focus on Patient Care
By entrusting billing processes to external experts, healthcare providers can redirect their focus and resources towards delivering high-quality patient care. With billing responsibilities offloaded, healthcare professionals can dedicate more time and attention to diagnosing and treating patients, enhancing the overall patient experience and satisfaction.
Avoid Errors Such as Overbilling and Underbilling
Billing companies employ coding experts and conduct regular audits to ensure accurate and compliant billing practices. These professionals meticulously review medical records, documentation, and coding practices to identify and rectify any instances of overbilling or underbilling.
By maintaining strict adherence to billing regulations and guidelines, billing companies help healthcare providers avoid costly compliance issues and penalties.
Secure Patient Data
Billing companies prioritize data security and confidentiality to protect sensitive patient information from unauthorized access, breaches, or cyber threats. They implement robust cybersecurity measures, encryption protocols, and access controls to safeguard patient data throughout the billing process.
By partnering with reputable billing companies, healthcare providers can ensure the privacy and integrity of patient information, building trust and confidence among patients.
Deeper Insight Into the Revenue Cycle
Outsourced billing services provide healthcare providers with comprehensive reports, analytics, and insights into their revenue cycle performance. These detailed reports highlight key performance metrics, trends, and areas for improvement, enabling healthcare organizations to make informed decisions and optimize their revenue cycle management strategies.
By gaining deeper insight into their revenue cycle, healthcare providers can identify opportunities to increase revenue, reduce costs, and enhance overall financial performance.
Different Types of Medical Billing Companies
Before choosing a company to outsource medical billing to, healthcare providers first need to be aware of types of the three types of medical billing companies.
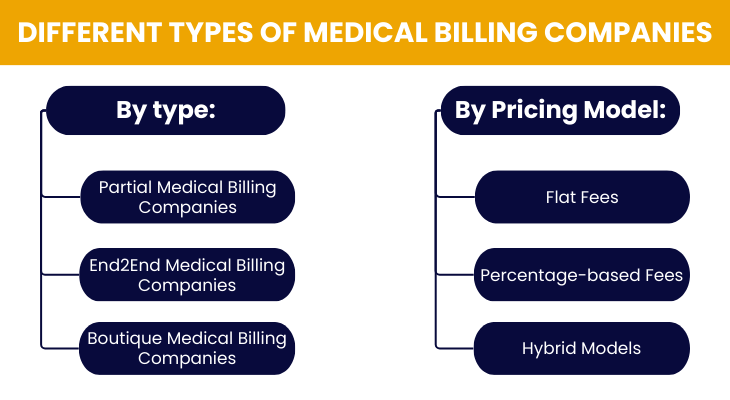
Partial Medical Billing Companies
These companies specialize in offering select services within the medical billing process. Typically, partial medical billing companies focus on specific aspects such as coding validation, claim submission, or handling rejections due to authorizations and eligibility.
By narrowing their focus to particular components of the billing process, these companies cater to the needs of healthcare practices that already have an in-house billing staff but require assistance with specific tasks. Partial medical billing companies provide targeted expertise and support, complementing the existing capabilities of healthcare organizations.
End-to-End Medical Billing Companies
End2End medical billing companies offer comprehensive billing services that cover the entire revenue cycle from start to finish. These companies handle all aspects of medical billing, including patient demographics, medical coding, charge entry, claims transmission, payment posting, accounts receivable follow-up, denial management, and more.
By providing end-to-end solutions, these companies streamline the billing process and ensure maximum efficiency and accuracy throughout the revenue cycle. Healthcare providers can benefit from outsourcing their billing needs to End2End companies, as they receive comprehensive support and expertise to optimize their financial performance.
Boutique Medical Billing Companies
Boutique firms specialize in serving specific medical specialties or niche practices, offering tailored billing solutions to meet the unique requirements of their clients. These companies leverage their expertise and understanding of specialized medical fields to provide customized billing services that align with the intricacies of each specialty.
Boutique medical billing companies may focus on areas such as orthopedics, cardiology, dermatology, or pediatrics, among others. By catering to the specific needs of niche practices, these firms deliver personalized attention, industry-specific knowledge, and specialized billing strategies that maximize revenue and operational efficiency for their clients.
Pricing Models for Outsourced Medical Billing
Another factor that healthcare organizations need to pay attention to while choosing a medical billing outsourcing partner is the fee structure or pricing model they use to charge for their services. Again, there are three styles of pricing that medical billing companies use.
Flat Fees
Flat fees refer to a pricing structure where a fixed amount is charged for each claim processed by the medical billing company. With flat fees, healthcare providers know exactly how much they will be charged for each billing transaction, providing predictability and transparency in costs.
This pricing model offers simplicity and ease of budgeting for healthcare practices, as they can anticipate their billing expenses with accuracy. Flat fees are often preferred by healthcare providers who value cost predictability and want to avoid unexpected fluctuations in billing expenses.
Percentage-based Fees
Percentage-based fees involve charging a percentage of the total amount collected by the medical billing company on behalf of the healthcare provider. In this pricing model, the billing company’s compensation is directly tied to the revenue generated for the healthcare practice.
By aligning the billing company’s pay with the revenue earned, percentage-based fees incentivize the billing company to maximize collections and optimize revenue performance for their clients. This pricing structure ensures that the billing company is motivated to achieve the best possible financial outcomes for the healthcare provider, as their compensation is directly linked to the success of the billing process.
Hybrid Models
Hybrid models combine elements of both flat fees and percentage-based fees, offering a flexible and customizable pricing structure that meets the unique needs of healthcare providers. In hybrid models, healthcare practices may pay a fixed fee for basic billing services, such as claim processing, while also paying a percentage of the revenue collected for additional services or higher-tier billing packages.
This hybrid approach provides healthcare providers with the benefits of both fixed costs and performance-based incentives, allowing them to tailor their billing expenses to their specific requirements and budget constraints. Hybrid models offer versatility and cost-effectiveness, making them an attractive option for healthcare practices seeking outsourced billing solutions.
Choosing the Best Medical Billing Company
Other than the type of company and the pricing model, here are some important factors healthcare organizations ought to consider before choosing a medical billing company to outsource to.
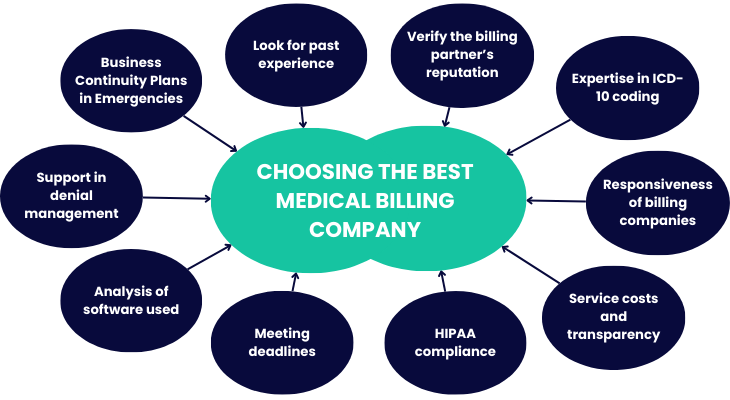
Look for past experience
Prioritize companies with extensive experience in medical billing, as they are more likely to have the expertise and resources necessary to handle your billing needs effectively. A track record of success indicates reliability and proficiency in navigating the complexities of medical billing.
Verify the billing partner’s reputation
Research the reputation of potential billing partners by reading client testimonials, reviews, and industry ratings. A reputable billing company will have positive feedback from satisfied clients, demonstrating their reliability and trustworthiness.
Expertise in ICD-10 coding
Ensure that the billing company is well-versed in the latest coding standards, particularly ICD-10, to ensure accurate and compliant billing practices. Proficiency in coding minimizes errors and reduces the risk of claim denials, ultimately maximizing reimbursement for healthcare services.
Responsiveness of billing companies
Choose a billing company that prioritizes responsive communication and support. Prompt responses to inquiries and proactive problem-solving are essential for addressing billing issues and ensuring smooth operations.
Service costs and transparency
Understand the billing company’s pricing structure and ensure transparency regarding fees, charges, and billing practices. Clear communication about costs helps avoid unexpected expenses and fosters a transparent partnership.
HIPAA compliance
Verify that the billing company adheres to HIPAA regulations to protect patient data and privacy. Compliance with HIPAA standards ensures the security and confidentiality of sensitive medical information, safeguarding both patient trust and legal compliance.
Meeting deadlines
Select a billing company capable of meeting deadlines consistently. Timely billing and reimbursement are critical for maintaining cash flow and financial stability. A reliable billing partner will prioritize deadlines and ensure the timely submission of claims.
Analysis of software used
Assess the software and technology utilized by the billing company to ensure compatibility, efficiency, and security. Advanced billing software can streamline processes, minimize errors, and enhance overall billing performance.
Support for denial management
Choose a billing company that offers robust denial management services to address claim denials promptly and effectively. Effective denial management maximizes revenue recovery and reduces revenue leakage, ensuring optimal financial outcomes for your practice.
Business Continuity Plans in Emergencies
Ensure that the billing company has comprehensive business continuity plans in place to maintain operations during emergencies, disruptions, or disasters. Preparedness for unforeseen events demonstrates reliability and ensures uninterrupted billing services, even in challenging circumstances.
Outsource Your Medical Billing to Promantra
Promantra has been at the forefront of RCM and has outsourced medical billing services since 2003. Along with more than two decades of experience, our HIPAA compliant team also boasts ISO 9001 and ISO 27001 certifications.
As an End-to-End service provider, our comprehensive medical billing solutions can be customized to suit your organization’s unique needs. Be it the use of the latest technology, constant training and upgrades, the application of Six Sigma to guarantee the quality of our processes or the access to reports and business intelligence that we offer, you can rest assured that your medical billing processes are in the best possible hands.
To learn more about the full scope of our RCM and medical billing services, get in touch with our team today!




