In the current dynamic healthcare environment, balancing the financial aspect and the quality of service delivery is necessary.
This is where revenue cycle management (RCM) analytics come into play. RCM analytics offer detailed information that assists healthcare organizations in increasing financial returns, operational efficiency, and patient satisfaction.
Knowing why RCM analytics are important can show how healthcare organizations can manage their revenues and make everything run more smoothly and efficiently.
What is Revenue Cycle Management Analytics?
Revenue cycle management (RCM) analytics uses data analysis tools and techniques to monitor, manage, and improve healthcare organizations’ financial processes.
These analytics include patient registration, insurance confirmation, billing, payment, and financial reporting.
Thus, RCM analytics use data to inform healthcare providers about areas of concern, errors, and how to optimize revenue.
Key Components and Stages Involved in RCM
RCM analytics encompasses several vital components and stages:
- Patient Registration and Scheduling: This initial stage involves collecting accurate patient information and scheduling appointments. Analytics help ensure data accuracy and streamline the registration process.
- Insurance Verification and Authorization: Verifying patient insurance coverage and obtaining necessary authorizations are critical to avoiding denied claims. RCM analytics identify potential issues before they become costly problems.
- Charge Capture: This stage involves accurately recording services provided to patients. Analytics ensure all billable services are captured, reducing revenue leakage.
- Coding and Documentation: Proper coding of services is essential for accurate billing. RCM analytics monitor coding practices to ensure compliance and optimize reimbursement.
- Claims Submission: Submitting claims to payers for reimbursement is a crucial step. Analytics track claim status and highlight trends in denials or delays, allowing for proactive resolution.
- Payment Posting: Once received, they must be accurately posted to patient accounts. Analytics help reconcile payments and identify discrepancies.
- Denial Management: Managing denied claims is vital for recovering lost revenue. RCM analytics analyze denial patterns and provide insights for preventing future denials.
- Patient Collections: Collecting payments from patients can be challenging. Analytics identify outstanding balances and optimize collection strategies.
- Reporting and Analysis: Finally, RCM analytics generate detailed reports on financial performance, providing a comprehensive view of the revenue cycle. These insights enable healthcare providers to make data-driven decisions and continuously improve their processes.
Importance of RCM Analytics in Healthcare
Let us have a look at why you should have revenue cycle management analytics in place as a healthcare organization:
Enhancing Financial Performance
Revenue cycle management analytics are essential in improving the financial position of healthcare institutions.
These analytics offer a detailed breakdown of the revenue cycle and give insights into maximizing revenue and minimizing costs.
For example, they can identify areas of waste in billing procedures, show trends in claims denial, and demonstrate areas of coding errors.
This level of visibility enables healthcare providers to make the right decisions to improve their financial status and get the highest possible reimbursement for their services.
Improving Operational Efficiency
Efficiency is essential in any healthcare facility, and RCM analytics are critical in attaining efficiency.
Analyzing data at different stages of the revenue cycle helps optimize healthcare facilities’ work, reduce the burden on employees, and minimize the number of mistakes.
For instance, RCM analytics can help in patient registration, insurance confirmation, and claims processing.
This not only helps shorten the revenue cycle but also reduces the burden on the staff and allows them to concentrate more on the patients. The end product is an operation that is smooth, efficient, and free from unnecessary hitches.
Ensuring Compliance and Risk Management
Healthcare regulations and risk management are critical in the healthcare industry. They ensure that all healthcare facilities operate legally and manage any risks that may arise.
Revenue cycle management analytics help maintain compliance by reviewing coding, documentation, and regulation changes.
These analytics can help foresee compliance risks that may become critical problems, thus minimizing the probability of audits and penalties.
Moreover, by analyzing trends and patterns, RCM analytics can assist healthcare organizations in managing risks, such as determining which areas are likely to experience claim denials or payment delays. This approach makes compliance and risk management part and parcel of the revenue cycle.
Key Benefits of Healthcare Revenue Cycle Management Analytics
Let us look at some of the benefits associated with RCM analytics:
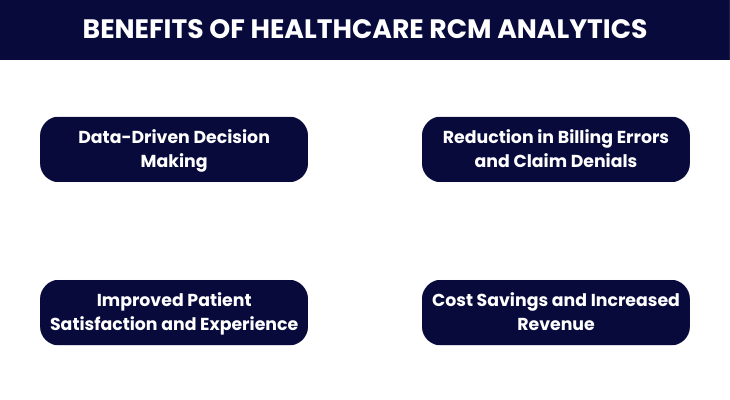
Data-Driven Decision Making
RCM analytics empower healthcare organizations with data-driven decision-making capabilities. By leveraging real-time data and comprehensive reports, healthcare providers can make informed choices that positively impact their operations and financial health.
Analytics help identify trends, forecast future revenue, and pinpoint improvement areas. This informed approach ensures that decisions are based on solid data rather than assumptions, leading to more effective strategies and outcomes.
Reduction in Billing Errors and Claim Denials
Billing errors and claim denials can significantly impact a healthcare organization’s revenue. RCM analytics are crucial in minimizing these issues by identifying common errors and denial patterns.
Healthcare providers can implement corrective measures to prevent future mistakes by analyzing data from past claims.
This proactive approach reduces the number of denied claims and ensures that billing processes are accurate and efficient, leading to faster reimbursements and improved cash flow.
Improved Patient Satisfaction and Experience
A smooth and efficient revenue cycle directly improves patient satisfaction and experience. RCM analytics streamline administrative processes, reducing wait times for appointments, billing, and payments.
When patients experience fewer billing issues and faster service, their overall satisfaction with the healthcare provider increases.
Additionally, accurate billing and clear communication about payment responsibilities enhance the patient experience, fostering trust and loyalty.
Cost Savings and Increased Revenue
By optimizing various aspects of the revenue cycle, RCM analytics lead to significant cost savings and increased revenue.
Analytics help identify inefficiencies, eliminate redundancies, and streamline processes, reducing operational costs.
The cost savings achieved through improved efficiency and the additional revenue from optimized billing processes contribute to the organization’s financial stability and growth.
Components of Effective Healthcare Revenue Cycle Analytics
Here are the major components of RCM analytics:
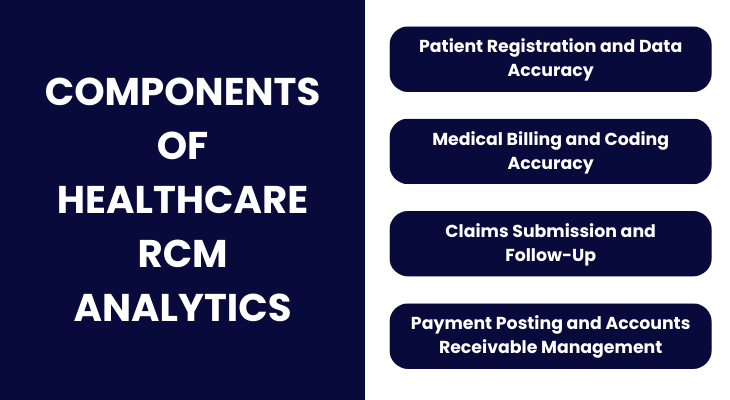
Patient Registration and Data Accuracy
The foundation of an efficient revenue cycle starts with accurate patient registration. Effective RCM analytics ensure that all patient data, including demographic details, insurance information, and contact details, are correctly entered and verified at the point of registration.
This accuracy reduces the likelihood of claim denials and billing errors. Analytics tools can identify discrepancies or missing information in real-time, prompting immediate corrections and maintaining data integrity.
Medical Billing and Coding Accuracy
Accurate medical billing and coding are crucial for maximizing revenue and ensuring compliance with regulations.
RCM analytics help monitor and improve coding accuracy by identifying common errors, tracking coding trends, and ensuring all billable services are correctly captured.
By analyzing coding practices and comparing them against industry standards, healthcare providers can minimize the risk of denied claims and enhance reimbursement rates.
Claims Submission and Follow-Up
Submitting claims accurately and promptly is essential for a smooth revenue cycle. RCM analytics streamline the claims submission process by automating checks for errors and ensuring that all necessary documentation is included.
These analytics also play a crucial role in follow-up activities by tracking the status of submitted claims, identifying delays, and flagging denied claims for quick resolution.
By providing insights into the claims lifecycle, revenue cycle management analytics help reduce the time it takes to receive payments and improve overall cash flow.
Payment Posting and Accounts Receivable Management
Effective payment posting and accounts receivable (AR) management is vital for maintaining a healthy revenue cycle.
RCM analytics facilitate accurate and timely posting of payments, ensuring that patient accounts reflect the latest transactions.
By analyzing payment patterns and AR data, healthcare providers can identify trends in payment delays or discrepancies, allowing them to take proactive measures to address issues.
Analytics also help prioritize follow-up actions on outstanding accounts, improving collection rates and reducing the amount of uncollected revenue.
How RCM Analytics Transforms Healthcare Organizations
Let’s look at this case study to see how revenue cycle management analytics aided healthcare:
Case Study: Enhancing Healthcare Efficiency with RCM Analytics
A leading molecular diagnostics company renowned for its groundbreaking cancer screening products sought to streamline its order entry process to boost efficiency and minimize operational backlogs.
They turned to Revenue Cycle Management (RCM) services to implement a robust order entry system, aligning with their commitment to providing seamless and timely patient care.
Challenges Encountered
The project faced several significant challenges during its implementation:
- Phased and Aggressive Transition: The company had a backlog of 90,000 orders, necessitating a simultaneous go-live for Phases 1 and 2. Coordinating 100 resources under these conditions posed a considerable challenge.
- Maintaining Quality with Increased Resources: Concerns about sustaining quality and accuracy were raised due to the increased resources required for the simultaneous go-live.
- Uneven Training Ratio: Initially, only ten users from operations were trained, creating an uneven trained-to-untrained staff ratio of 1:10.
Solutions Implemented
RCM services addressed these challenges with the following strategic solutions:
- Team Segregation: The team was divided based on strengths and responsibilities, with one group focusing on order entry and the other on document reindexing.
- Comprehensive Training: Phase 3 users were trained proactively, utilizing feedback and innovative micro-learnings from the first two groups.
- Regular Client Interaction: Daily touch base calls were established to facilitate collaboration and resolve issues promptly.
Results Achieved
The implementation of RCM analytics led to significant improvements:
- Exceeded Productivity Targets: The team achieved over 100% of the Statement of Work (SOW) target production from the first week.
- Backlog Clearance: By the first week of January 2023, the entire backlog of 90,000 orders was cleared, streamlining operations.
- Client Acknowledgment: The client appreciated the progress and expressed interest in transitioning additional processes later in the year.
Conclusion
This case study underscores the transformative power of Revenue Cycle Management (RCM) analytics in the healthcare industry.
By leveraging advanced analytics, RCM services enhanced operational efficiency, maintained high-quality standards, and significantly reduced order backlogs.
The successful implementation not only met but exceeded client expectations, demonstrating the critical role of RCM analytics in optimizing healthcare operations and ensuring timely patient care.
Tools and Technologies Used in RCM Analytics
- AI and Machine Learning: For predictive analytics, billing accuracy, and identifying revenue leakage points.
- Robotic Process Automation (RPA): To automate repetitive tasks in billing and claims management.
- Real-time Data Analytics: To monitor and improve patient registration, billing, and compliance processes.
Best Practices for Implementing RCM Analytics
- Data Integration: Ensure seamless integration of RCM analytics tools with existing healthcare IT systems.
- Continuous Monitoring: Regularly monitor key performance indicators (KPIs) and adjust strategies based on real-time data insights.
- Training and Education: Provide ongoing training for staff on new technologies and processes.
- Collaboration: To align goals and improve efficiency, Foster collaboration between IT, finance, and clinical departments.
Challenges in Implementing RCM Analytics
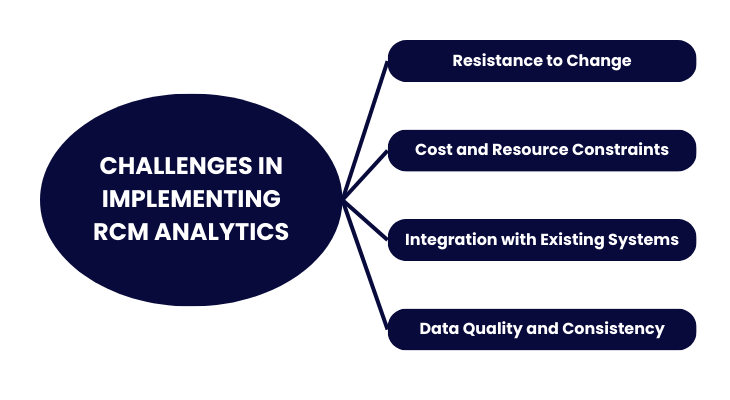
Data Quality and Consistency
Ensuring the accuracy and consistency of data across various systems is a significant challenge. Consistent data can lead to correct insights and better decision-making.
Solution: Implement data governance practices to standardize data entry procedures and utilize data cleaning tools to maintain data quality.
Resistance to Change
Healthcare staff may resist new analytics tools and processes because they need to familiarize themselves with them or fear job displacement.
Solution: Engage staff early in the implementation process, provide clear communication about the new system’s benefits, and offer extensive training to ease the transition.
Integration with Existing Systems
Integrating RCM analytics with existing healthcare IT systems can be complex and time-consuming.
Solution: Choose analytics tools compatible with current systems and employ integration experts to ensure a smooth transition.
Cost and Resource Constraints
Implementing advanced RCM analytics can require significant financial and human resources, which may be a barrier for smaller healthcare providers.
Solution: Start with scalable solutions that can grow with the organization and seek out vendors offering flexible pricing models or partnerships.
Importance of Training and Education
Training and education are crucial to the successful implementation of RCM analytics. Staff must be proficient in using new tools and understanding the insights derived from analytics.
Continuous education ensures that staff stay updated on best practices and evolving technologies.
- Initial Training: Comprehensive training sessions should be conducted during the implementation phase to familiarize staff with the new system.
- Ongoing Education: Regular workshops and refresher courses help maintain a high level of competence and adapt to any updates or changes in the system.
- Certification Programs: Encourage staff to pursue relevant certifications to deepen their knowledge and skills in RCM analytics.
Integration with Existing Systems
Effective integration of RCM analytics with existing healthcare IT systems is critical for seamless operations. This involves:
- Interoperability: Ensure the new analytics tools can communicate and share data with existing systems.
- Data Migration: Develop a robust plan for migrating historical data to the new system without loss or corruption.
- Custom Solutions: Tailor the integration process to address the specific needs and workflows of the organization.
Future Trends in RCM Analytics
AI and machine learning are revolutionizing RCM analytics by providing advanced capabilities such as:
- Predictive Analytics: This method uses historical data to predict future trends, such as patient volumes and revenue cycles, enabling proactive management.
- Automated Processes: AI can automate routine tasks like billing and coding, reducing errors and freeing up staff for more strategic activities.
- Enhanced Data Insights: Machine learning algorithms can uncover hidden patterns and correlations in large datasets, leading to more informed decision-making.
Predictive Analytics and Real-Time Data Processing
Predictive analytics and real-time data processing are becoming increasingly vital revenue cycle management analytics. These technologies enable healthcare providers to:
- Forecast Revenue Trends: Predict future cash flows and identify potential financial challenges before they arise.
- Monitor Performance: Real-time data processing allows for continuous monitoring of key metrics, facilitating timely interventions.
- Improve Patient Outcomes: Healthcare providers can enhance care delivery and efficiency by predicting patient needs and resource utilization.
Evolving Regulatory Requirements and Compliance
The regulatory landscape for healthcare is continually changing, posing challenges for RCM analytics. Future trends include:
- Compliance Automation: Tools that automatically update and comply with the latest regulations, reducing the burden on staff.
- Regulatory Reporting: Advanced analytics can streamline reporting to regulatory bodies, ensuring accuracy and timeliness.
- Security Enhancements: As data privacy laws evolve, RCM analytics will increasingly incorporate advanced security measures to protect patient information.
Summing Up
Revenue Cycle Management (RCM) analytics are essential for transforming the healthcare industry. By utilizing data-driven insights, healthcare organizations can enhance financial performance, improve operational efficiency, and ensure compliance.
Effective RCM analytics reduce billing errors, minimize claim denials, and boost patient satisfaction, leading to increased revenue and cost savings.
Embracing RCM analytics enables healthcare providers to navigate a complex environment with greater transparency and efficiency, ensuring better patient care and financial stability.
Revolutionizing Healthcare Revenue Cycle Management with ProMantra
In today’s healthcare landscape, providers face mounting challenges in documentation, compliance, reimbursements, and staffing shortages.
ProMantra offers a solution by providing transparency and efficiency in revenue cycle management. ProMantra allows providers to streamline their billing processes, reduce errors, and improve financial outcomes.
Ready to transform your revenue cycle management? Contact ProMantra today to learn how we can help your organization thrive.




