Healthcare providers have a dual focus: delivering excellent patient care and maintaining financial health. Revenue Cycle Management (RCM) is the process that bridges these two priorities.
But what is RCM, and why is it vital in the healthcare industry? In essence, RCM ensures that healthcare businesses get paid for their services, managing everything from patient registration to the final payment.
The healthcare revenue cycle is one of the crucial aspects of the healthcare industry and hence it is pivotal to understand its significance.
In this blog, we’ll explore the basics of RCM and its critical role in keeping healthcare organizations financially sound.
What is Revenue Cycle Management?
RCM or Revenue Cycle Management is the main support of financial processes in the healthcare industry.
In its simplest form, RCM is the mechanism that healthcare organizations employ in managing patient care cycles from registration and appointment scheduling to the last point of payment for outstanding balances.
It is all about making sure that the services offered are billed correctly and reimbursed in the right manner.
RCM is not only billing but a system that covers the financial process of patient care. The goal of RCM is to optimize the activities that are connected with revenue production, including insurance pre-certification, coding and claims follow-up.
Revenue cycle management is the process through which healthcare organizations can reduce cycles, avoid mistakes, and be paid fairly for their services.
Key Components of RCM
The revenue cycle is made up of several key components that work together to ensure smooth financial operations:
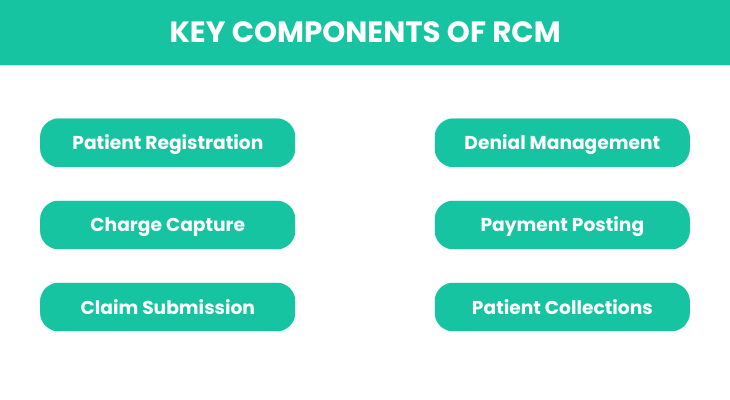
- Patient Registration: Collecting and verifying patient information, including insurance details.
- Charge Capture: Accurately documenting the services provided to patients for billing purposes.
- Claim Submission: Preparing and sending claims to insurance companies for payment.
- Denial Management: Addressing and correcting any claims that insurers deny.
- Payment Posting: Recording payments received from insurers and patients.
- Patient Collections: Following up on outstanding balances owed by patients.
The Healthcare Revenue Cycle
The healthcare revenue cycle is a complex process that starts from the time when a patient makes an appointment.
Patient registration, diagnosis, treatment, prescription, administration of drugs, and payment are all part of this cycle and all are important in making sure that those who offer healthcare services are paid for their services.
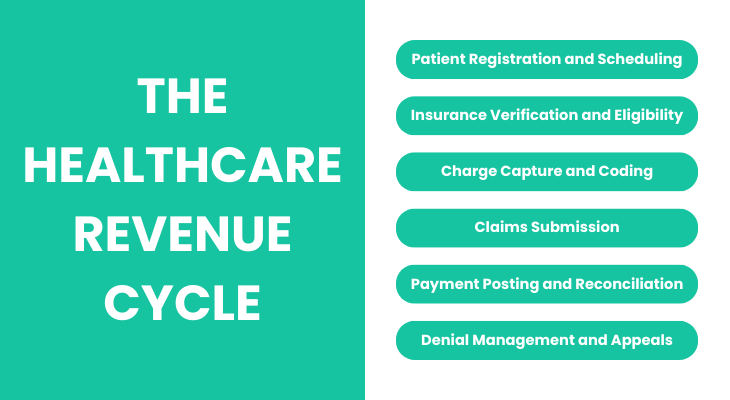
Patient Registration and Scheduling
The first process in the revenue cycle is the registration and scheduling where a patient’s details and insurance details are taken.
Data entry is important at this stage because any mistake made will cause a problem in the future like denial of a claim or delayed payment.
It also helps in the right planning of resources so that there are no gaps in the services being offered and at the same time, there is optimization of the revenue streams.
Insurance Verification and Eligibility
The other crucial process that follows the registration of a patient is insurance verification and eligibility. It is crucial to verify the insurance status and ensure that the services that are going to be delivered are within the insurance coverage before any service is delivered.
This step is useful in avoiding extra charges to patients and also minimizes the chances of claim rejection by the healthcare provider.
Pre-certification of services helps healthcare organizations avoid billing hassles and increase the chances of receiving payments on time.
You Might Also Like – Why Revenue Cycle Management Analytics Are Crucial for Healthcare Organizations
Charge Capture and Coding
The next process of the revenue cycle after a healthcare service is rendered is charge capture and coding.
This includes writing down all the services and procedures that a patient undergoes during his or her visit. Every service has a code and it is used to inform the insurance companies on what was done to the patient.
The reason why coding has to be done correctly is that even a single error can result in claim rejection or lower payment.
Accurate charge capture means that all services offered are recorded, thus increasing the chances of the healthcare provider earning more revenue.
Check Out The Steps for Accurate Medical Coding: A Comprehensive Guide
Claims Submission
Once the charges are captured and coded, the next step is claims submission. This involves sending the detailed claim to the patient’s insurance company for payment.
The claim must be accurate and complete to avoid delays or denials. Timely submission of claims is crucial, as insurance companies often have strict deadlines.
A well-organized claims submission process helps ensure payments are received as quickly as possible, keeping the revenue cycle smoothly.
Payment Posting and Reconciliation
The payment process starts after the claim has been submitted and granted. Payment posting and reconciliation entail the entry of the amount received from insurance companies and patients into the health care providers’ accounts.
This step makes sure that the payments made correspond to the billed amount and also helps to identify the differences.
Proper payment posting is very important in ensuring that the financial records are clean and that the healthcare provider is paid for all the services offered.
Denial Management and Appeals
However, even if there is a well-developed process in place, claim denials are still inevitable. Appeals and denial management are about handling these problems outright.
When a claim is denied it is necessary to find out why and correct the situation as soon as possible. This may include filing for a reconsideration of the claim with more evidence or appealing the decision if the denial appears to be unfair.
Denial management leads to revenue recovery and better submission of future claims since it establishes the causes of the denials.
Challenges in Revenue Cycle Management
Revenue cycle management is a crucial process in healthcare and like any other process, it has its own set of challenges.
In this case, even small mistakes can result in huge losses; it is therefore important for healthcare providers to be sensitive to such problems and try to avoid them.
Common Billing Errors
A common problem that is often encountered in RCM is that of billing errors. These can include wrong patient data, coding errors, billing and coding duplication, and lack of documentation.
Slight mistakes can result in claims being denied or payment being delayed and this can greatly affect cash flow.
To healthcare providers, it is crucial to reduce billing errors since claims have to go through various processes before payments are received.
Impact of Denials on Revenue
Other significant barriers to the revenue cycle include denials. When a claim is denied, the healthcare provider is not being compensated for the services that he or she has already offered.
This can have a direct impact on the revenues and it will be on the negative side. Not only does the claim end up being denied and therefore not paid, but it also means that more money has to be spent to fix the mistake and resubmit the claim.
Denial rates can greatly impact a healthcare organization’s financial health and thus proper denial management is vital for the organization’s cash flow.
Strategies to Optimize RCM
Due to the high level of complexities involved in Revenue Cycle Management, it is important to have efficient strategies to be put in place to support the process.
There are two major areas that have the potential for improvement in the healthcare providers and these are technology and interprofessional team communication.
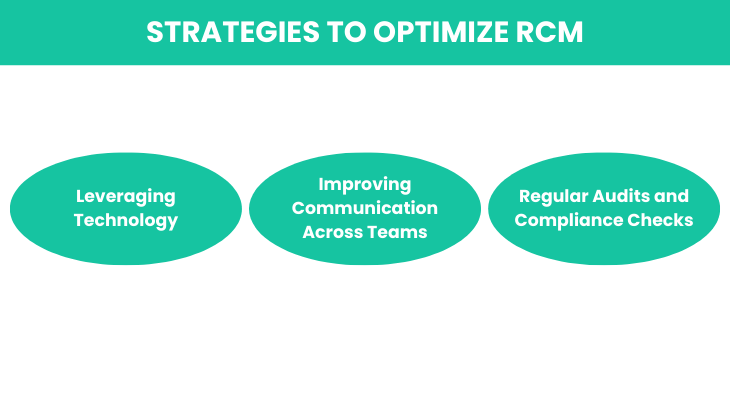
Leveraging Technology
Technology can be considered as the key driver for the improvement of RCM. Numerous software solutions can help in the automation of revenue cycle management from registration, charge entry, coding, claims submission, and payment posting.
Such tools assist in minimizing human mistakes, automating processes, and giving real-time analysis of the business’s financial position.
For example, automated coding systems can guarantee that they are correct, and predictive analytics can assist in discovering problems before they escalate.
The implementation of technology in the field of healthcare can go a long way in enhancing the revenue cycle in the healthcare providers’ field, thus cutting costs and improving efficiency.
Improving Communication Across Teams
Another key component of the revenue cycle is communication. RCM is a process that affects many departments in a healthcare facility such as the patient services, billing, coding, and finance departments.
When these teams operate independently of each other, there is a communication breakdown, time wastage, and mistakes.
Enhancing communication between the teams ensures that all the members are aware of the various problems that may be prevalent hence making it easier to address them.
It is possible to improve collaboration, which translates to a more efficient revenue cycle and a healthier bottom line by having regular meetings, using the same platforms, and setting up clear protocols.
Regular Audits and Compliance Checks
It is important to note that periodic audits and compliance checks are essential to the overall integrity of the revenue cycle.
Through regular billing practice and regulatory compliance audits, healthcare providers can detect problems that may exist and address them before they become bigger problems.
Audits assist in confirming that coding is correct, claims are well documented and payments are properly recorded.
Moreover, maintaining compliance with healthcare regulations reduces the probability of incurring fines and increases the credibility of the organization.
Audits do not only protect revenue but also help to maintain the company’s financial stability in the long run.
Learn Effective Strategies to Improve Revenue Cycle Management
Benefits of Effective RCM
Apart from the financial benefits, there are several advantages of putting in place a good RCM system.
When RCM is improved, healthcare providers can realize better financial returns, satisfied patients, and low operating expenses.
Enhanced Financial Performance
Another advantage of good RCM is that it helps in the enhancement of the financial status of the organization.
A good revenue cycle means that the claims are processed correctly and on time hence leading to quick reimbursement and few rejections.
This steady and predictable cash flow helps healthcare providers plan their finances well, invest in new technologies, and develop their services.
The reduction of billing errors and the enhancement of the processes involved in billing also aid in the optimization of the revenues and the minimization of the losses of the organization.
Improved Patient Satisfaction
It is important to note that effective RCM is about improving the company’s revenues and increasing patient satisfaction.
An efficient revenue cycle lowers the incidences of billing mistakes. It makes it possible for the patients to be charged the right amount at the right time hence minimizing billing issues.
Also, when administrative procedures are streamlined, healthcare providers can devote their time to enhancing the quality of service delivery and the relationship with patients.
Patients like to know what is going on and being able to explain it to them is one of the benefits of an optimized RCM system.
Reduced Operational Costs
The other important advantage of good RCM is the cutting down of operational costs. This means that healthcare providers can minimize the need to undertake manual interventions hence cutting on the costs of labor and at the same time minimizing the possibility of costly errors.
Effective RCM practices also reduce the time staff spends on administrative work, which means they are not overwhelmed with mundane tasks that take up much of their time.
This in turn results in a lean organization where resources are used appropriately to enhance patient care and other areas of importance.
Summing Up
Effective Revenue Cycle Management is crucial for healthcare organizations striving to maintain financial health and deliver quality patient care.
By optimizing the revenue cycle—from patient registration to denial management—healthcare providers can enhance their financial performance, reduce operational costs, and improve patient satisfaction.
In an industry where precision and efficiency are key, investing in a robust RCM system is not just beneficial; it’s essential for long-term success.
Promantra: Your Trusted Partner in RCM
Promantra offers tailored Revenue Cycle Management (RCM) solutions designed to meet the unique needs of healthcare organizations.
From medical billing and coding to denial management and payment posting, we help you streamline your operations, improve cash flow, and reduce costs.
Reach out to Promantra today to learn how our RCM services can optimize your financial performance and support your success.