Accurate medical billing plays a critical role in the financial health of emergency departments, especially with the frequent updates to CPT codes. According to the 2025 CPT code set, there are 420 overall changes, including 270 new codes, 112 deletions, and 38 revisions, highlighting the importance of staying up to date.
One of the most commonly used codes in emergency care is CPT code 99283, which is billed for moderate-complexity emergency department visits that require a detailed examination and medical decision-making.
In this blog, you’ll learn what CPT code 99283 covers, the key components needed for proper billing, and the common services it includes. We’ll also share tips for clear documentation, factors affecting it, how to avoid billing mistakes, the impact of modifiers, and best practices to keep your emergency billing accurate and efficient.
But before we get into all the details, let’s take a quick look at the basics.
What is CPT Code 99283?
CPT code 99283 refers to a Level 3 emergency department visit that requires a detailed history, a thorough examination, and medical decision-making of moderate complexity. You can use this code when a patient presents with a condition that is not immediately life-threatening but still requires careful evaluation and treatment. Common examples include moderate pain, mild to moderate respiratory issues, or injuries that need more than basic care.
You now know what CPT code 99283 is, but to get the most out of this code, it’s important to understand the components involved in billing it. Let’s explore what you need to pay attention to for successful claims submission.
Key Components Required for Billing 99283
To bill CPT code 99283 correctly for an emergency department visit, your documentation must clearly support key components. These components must be met to ensure your billing is accurate and compliant:
1. Expanded Problem-Focused History
You need to document a thorough account of the patient’s current condition, including their chief complaint, history of present illness, and a review of systems. Be sure to include relevant past medical, family, and social history that directly relates to the issue at hand.
2. Expanded Problem-Focused Examination
A focused physical exam is required, covering the affected body area(s) or organ system(s) connected to the patient’s complaint. Your documentation should include vital signs and any abnormal findings that are relevant to the reason for the visit.
3. Medical Decision Making of Moderate Complexity
Your documentation must reflect that the medical decision-making involved moderate complexity. This means you’ve evaluated the patient’s condition, possibly ordered diagnostic tests, and created a treatment plan that could involve low-risk interventions or follow-up care. This is common for moderate-severity issues like mild respiratory distress or acute abdominal pain.
4. Bundled Services
CPT 99283 includes certain bundled services, such as minor procedures, lab tests, imaging, counseling, and care coordination. These services are part of the visit and should not be billed separately.
Also Read: Medical Coding vs Medical Billing: Know the Difference
Even when you’ve done everything right during the visit, missing or unclear notes can lead to denied claims. That’s why proper documentation is just as important as the treatment itself.
Documentation Tips for Accurate CPT 99283 Billing
Accurate documentation is key to ensuring proper reimbursement for emergency department visits billed under CPT code 99283. Here are some essential tips to help you maintain clear, detailed, and compliant records.
- Capture the Chief Complaint Clearly: Always document the patient’s reason for the emergency visit in their own words. This is essential to justify the need for a moderate-complexity evaluation.
- Ensure Complete and Legible Records: Make sure your documentation is thorough, legible, and includes dates and times. Be clear and specific about what was done and why.
- Align with CMS and Payer Guidelines: Ensure that your documentation supports the moderate complexity required for CPT 99283 and aligns with Medicare and private payer guidelines to avoid denials.
- Support the Level of Service: Your documentation should clearly explain why the visit qualifies as a level 3 emergency service. Lack of detail can lead to downcoding or claim rejections.
- Update and Review Regularly: Stay up to date with coding changes and payer policies to ensure compliance and maximize reimbursement. Regularly reviewing your documentation practices will help maintain accuracy.
While accurate documentation is key to your billing process, understanding how and when to use modifiers can further fine-tune your claims. Modifiers can make all the difference in how your services are reimbursed, so it’s worth knowing when to apply them.
Modifier Uses for CPT 99283 Billing
Modifiers are essential when billing for emergency department visits with CPT code 99283, as they provide extra details about the services provided, ensuring your claims are accurate, compliant, and less likely to be denied.
Proper use of modifiers helps clarify the nature of the visit and supports correct reimbursement for the services rendered. The most commonly used modifiers for CPT 99283 are:
1. Modifier 25
Use Modifier 25 when a separate and significant evaluation and management (E/M) service is performed on the same day as another procedure.
For example, if you perform a 99283 visit and also conduct an EKG or X-ray during the same encounter, Modifier 25 shows that the E/M service was separate and necessary. This modifier is often required to avoid claim denials when both an E/M service and a procedure are billed together.
2. Modifier 57
Use Modifier 57 when the E/M service results in the decision to perform a major procedure, either on the same day or the next.
For example, if you see a patient for a 99283 visit and decide to admit them for surgery, Modifier 57 indicates that the E/M service led directly to the decision for surgery. This is important for proper reimbursement, especially for procedures with a 90-day global period.
Modifiers can certainly make your claims more accurate, but billing errors can still slip through the cracks. Let’s take a look at the factors affecting CPT code 99283.
Factors Affecting CPT Code 99283 Usage and Payment
When you bill for Emergency Department (ED) services, using CPT Code 99283 correctly is essential for getting paid accurately. This code represents a moderate-level Evaluation and Management (E/M) service. Here are 3 key factors that affect its use and payment:
1. Medical Decision-Making (MDM) Complexity
The level of medical decision-making (MDM) plays a big role in choosing the right E/M code. For CPT 99283, the MDM should be moderate, meaning the case involves multiple diagnoses or management options, moderate risk, or moderate complexity in reviewing data.
2. Documentation
Good documentation is key. You’ll need to include a clear history, exam, and detailed explanation of your decision-making process. Without enough documentation, you might face claim denials or lower payment, which means your service could be downcoded to a less complex level.
3. Insurance Payer Guidelines
Different insurance companies may have specific rules for CPT 99283. It’s important to check with each payer to understand their specific guidelines, so you’re always in line with what they expect.
Once you’re familiar with the factors affecting the use and payment of CPT Code 99283, it’s important to take a closer look at some common billing challenges and how to overcome them.
Common Billing Errors with CPT Code 99283
When billing for emergency department visits with CPT code 99283, even small mistakes can lead to claim denials, payment delays, or compliance problems. Below are some common errors with solutions:
1. Incorrect Place of Service (POS) Coding
CPT 99283 is only valid for emergency department services. Using it for visits in other settings, like an office Place of Service (POS) 11, can result in claim denials or payment delays.
How to avoid: Always check that you’re using POS 23 when billing for emergency visits. Train your team to apply the correct POS code for each claim.
2. Misuse or Overuse of CPT Code 99283
Using 99283 for visits that don’t meet the criteria can result in audits, denials, or accusations of upcoding.
How to avoid: Only use 99283 when the visit truly meets the moderate severity and complexity requirements. Review CPT guidelines regularly and educate your team on proper code selection.
3. Incorrect or Outdated Codes and Modifiers
Submitting claims with outdated or incorrect codes, or missing necessary modifiers, can lead to claim rejections.
How to avoid: Update your billing software and forms every year with the latest codes. Double-check that you’re using the most current CPT and ICD-10 codes and the right modifiers for each payer.
4. Diagnosis Code Errors
Using vague or incorrect diagnosis codes can cause claim denials.
How to avoid: Always use the most specific diagnosis code available. Review payer guidelines and update your forms annually to reflect the latest diagnosis codes.
5. Duplicate Billing
Submitting the same claim more than once, or using multiple E/M codes for the same visit, can result in denials or audits.
How to avoid: Use a reliable system in place to catch duplicate claims before they go out. That’s where having expert support can really help. ProMantra offers professional medical coding services to ensure every procedure and diagnosis is coded correctly the first time. This reduces the risk of duplicate billing, keeps your claims clean, and helps you get reimbursed faster without unnecessary setbacks.
6. Provider Number and NPI Issues
Incorrect or missing provider numbers or NPIs can delay payments or lead to claim rejections.
How to avoid: Ensure all provider information is accurate and up-to-date in your billing system. Verify NPIs and group numbers before submitting claims.
Also Read: The Consequences of Incorrect Medical Coding
Avoiding these billing errors is key, but there are also specific practices that can improve your billing workflow. Let’s take a closer look at the best practices for efficient emergency department billing.
Best Practices for Efficient Emergency Department Billing
Applying best practices to billing in the emergency department, especially when using CPT code 99283, can speed up reimbursement, reduce denials, and keep your practice in line with payer rules. Here is how to improve your billing process:
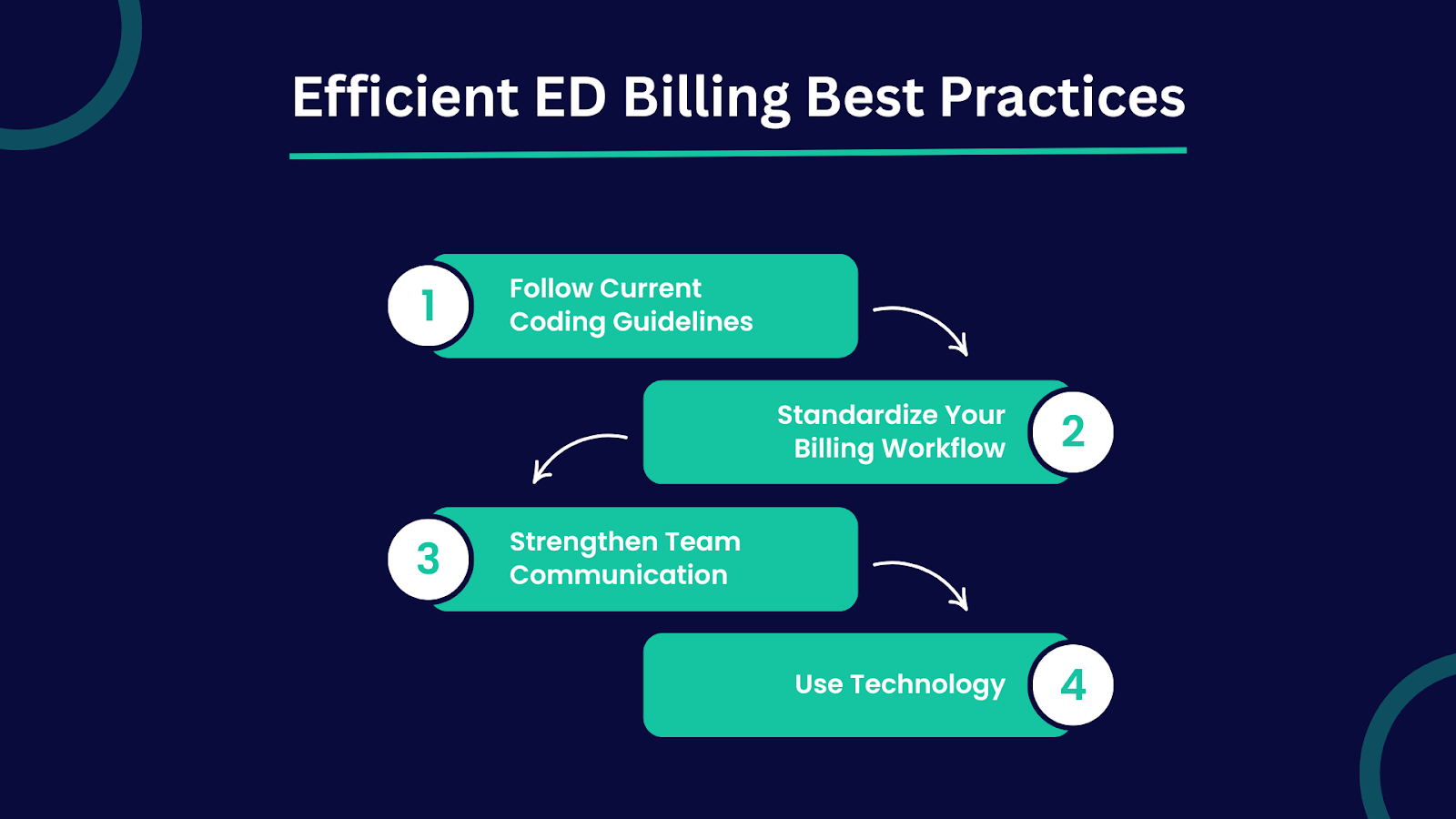
1. Follow Current Coding Guidelines
Use CPT code 99283 only when the visit meets moderate complexity criteria. To avoid rejections, assign the correct place of service code (usually POS 23). Stay updated with coding changes from the American Medical Association (AMA) and individual payers to ensure your claims are always accurate.
2. Standardize Your Billing Workflow
Creating clear and consistent billing processes across your team reduces errors and helps maintain compliance. It also improves efficiency, making it easier to train staff and submit clean claims.
3. Strengthen Team Communication
Encourage regular communication between providers and billing staff. This ensures that documentation supports coding and that any issues are addressed quickly. Periodic training helps your team stay aligned and updated on billing practices.
4. Use Technology
Automated billing systems can catch mistakes before claims go out. You can also consider outsourcing to a billing company that specializes in emergency medicine. These tools and services reduce administrative burden and support faster, more accurate reimbursements.
That’s why many healthcare providers trust ProMantra, which supports your practice with reliable, end-to-end solutions:
- Medical Coding: ProMantra ensures all medical procedures and diagnoses are coded correctly, helping you avoid claim errors and meet compliance standards.
- Medical Billing: ProMantra manages the full billing process, from creating accurate claims to submitting them to insurance companies, so you get paid faster with fewer delays.
- LTC Pharmacy Billing: For long-term care facilities, ProMantra provides specialized pharmacy billing services that ensure timely and accurate reimbursements.
Conclusion
Accurate coding is key to smooth and timely emergency department billing, especially when using CPT code 99283. It helps you avoid claim denials, ensures proper reimbursement, and keeps your billing process running efficiently.
If you’re looking for support in managing your medical coding and billing, ProMantra is here to help. ProMantra offers specialized healthcare services with a strong focus on medical coding and billing.
ProMantra ensures that your procedures and diagnoses are coded correctly, thereby reducing errors and delays in claims. Our team also verifies patient insurance before services are delivered, helping you avoid rejections and speed up reimbursements.To simplify and ensure the accuracy of your billing process, contact ProMantra’s expert team today.




