Healthcare RCM Services
Did you know that over 30% of all healthcare claims submitted in the US are denied initially? This translates to significant revenue loss for healthcare providers and added administrative burden. In today’s competitive healthcare environment, optimizing Revenue Cycle Management (RCM) is no longer optional – it’s essential for financial stability and delivering quality patient care.
This introduction presents a startling statistic about claim denials, a common challenge in healthcare RCM (RCM revenue cycle management). It then emphasizes the importance of RCM for financial health and patient care, piquing the reader’s interest in learning more.
Revenue Cycle Management (RCM) refers to the entire RCM process—the complex series of steps involved in collecting payment for healthcare services delivered. This process encompasses everything from patient registration and insurance verification to coding, billing, claims submission, and collecting patient payments or reimbursement from insurance companies. Inefficiencies in any stage of the RCM process can lead to delays, errors, and denials, jeopardizing your organization’s financial health.
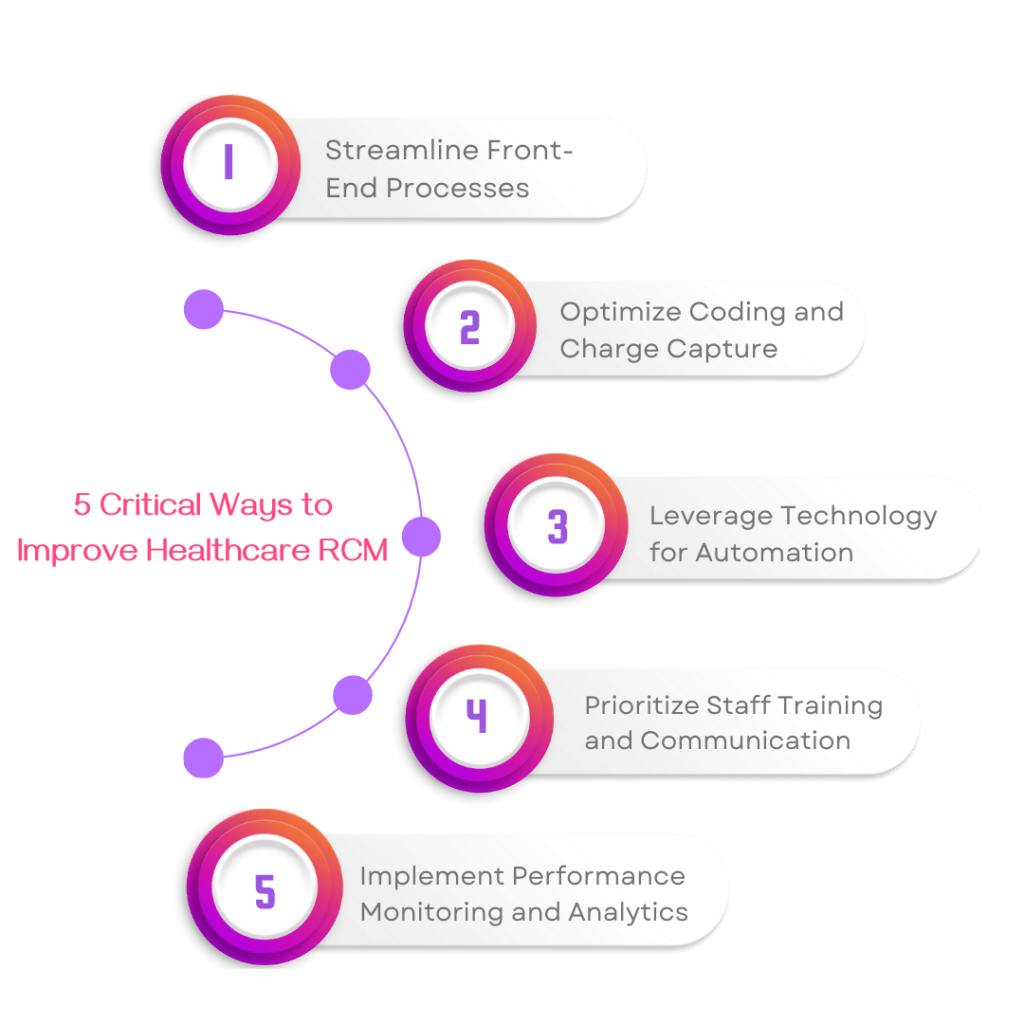
Fortunately, there are effective strategies healthcare providers can implement to streamline their RCM and maximize revenue capture. Here at ProMantra, we recommend five critical ways to optimize your RCM revenue cycle management:
- Streamline Front-End Processes: To minimize denials ensure accurate patient registration and insurance verification from the beginning.
- Optimize Coding and Charge Capture: Implement best practices and leverage technology to ensure accurate coding and capture all billable services.
- Leverage Technology for Automation and Efficiency: Automate repetitive tasks like claims submission and follow-up to improve efficiency and reduce errors.
- Prioritize Staff Training and Communication: Invest in training on RCM best practices and foster clear communication for a smoother workflow.
- Implement Performance Monitoring and Analytics: Track key RCM metrics to classify areas for improvement and optimize your revenue cycle.
The complexities of RCM can be particularly challenging for US healthcare providers facing:
- Staff Shortages: Finding and retaining qualified RCM personnel can be a significant hurdle.
- Regulatory Changes: Keeping up with ever-evolving healthcare regulations adds another layer of complexity.
- Technology Integration: Implementing and maintaining effective RCM technology can be costly and time-consuming.
Understanding these challenges, We offers a comprehensive suite of RCM solutions tailored to the specific needs of US healthcare providers. We leverage proven methodologies, industry expertise, and innovative technology to streamline your RCM processes, maximize revenue capture, and free up your staff to focus on what matters most – delivering quality patient care.
Critical Way #1: Streamline Front-End Processes: RCM in medical billing
Streamlining your front-end processes is the foundation of a smooth and efficient revenue cycle. This crucial stage encompasses patient registration, insurance verification, pre-appointment communication, and cost transparency. Errors and inefficiencies at this point can lead to significant delays, denials, and, ultimately, lost revenue for your healthcare organization.
The Importance of Accuracy:
Accurate patient registration and insurance verification are the cornerstones of minimizing denials in the RCM in the medical billing process. Here’s why:
- Only complete or accurate patient information: Please include data like demographics, insurance details, or co-pay amounts to ensure claims processing and avoid denial.
- Incorrect insurance verification: Unaware of patient coverage, deductibles, or prior authorizations can result in claims being rejected by insurance companies.
Strategies for Streamlining Front-End Processes:
Here are some key strategies to ensure accurate front-end processes:
- Invest in user-friendly registration systems: Implement electronic health record (EHR) systems with pre-populated fields and automated insurance verification tools.
- Train staff on best practices: Provide your registration and billing staff with comprehensive training on accurate data collection, insurance verification procedures, and understanding common errors to avoid.
- Standardize processes: Develop clear and consistent protocols for patient registration and insurance verification to ensure everyone follows the same steps.
- Implement online patient portals: These portals should allow patients to securely update their demographic and insurance information online, reducing errors and improving efficiency.
Pre-Appointment Communication and Cost Transparency:
Setting clear expectations with patients upfront can significantly improve your revenue cycle. Consider these strategies:
Pre-appointment communication:
Contact patients beforehand to confirm their appointment, gather necessary information, and discuss potential out-of-pocket costs based on their insurance coverage.
Cost transparency tools:
Provide patients with online calculators or clear explanations of potential charges related to specific procedures. This empowers them to make informed decisions and reduces billing surprises.
How ProMantra Can Help:
We understand the complexities of front-end RCM processes. We offer a wide range of solutions options that can help you streamline your workflows and improve accuracy:
- Technology expertise: ProMantra can help you select and implement user-friendly EHR systems and automated insurance verification tools to minimize errors.
- Staff training and support: Our training programs can equip your staff with the latest RCM best practices, ensuring efficient data collection and insurance verification procedures.
- Patient engagement solutions: We can assist you in developing online patient portals and implementing transparent communication strategies to improve patient experience and reduce billing disputes.
By investing in streamlining your front-end processes, you can establish a strong foundation for a more efficient and profitable RCM system. ProMantra can be your reliable partner in achieving this objective.
Critical Way #2: Optimize Coding and Charge Capture
Accurate and efficient coding lies at the heart of a successful revenue cycle. Proper coding ensures you capture all billable services rendered during a patient encounter, leading to timely and appropriate reimbursements from insurance companies. However, medical coding is a complex and ever-evolving field. Optimizing your coding practices within the RCM process is essential for maximizing revenue and minimizing lost opportunities.
The Impact of Proper Coding:
Inaccurate or incomplete coding can have significant repercussions for your healthcare organization:
Denial of claims:
Incorrect coding is a significant reason insurance companies deny claims. This translates to lost revenue and the added burden of fighting denials.
Delayed reimbursements:
Even minor coding errors can delay claim processing, leading to longer wait times for reimbursements and impacting your cash flow.
Missed revenue capture:
Under coding, or failing to capture all billable services, means you’re leaving money on the table.
Best Practices for Medical Coding:
Here are some essential best practices to ensure accurate and efficient coding in your RCM process:
- Stay up-to-date with coding regulations: Medical coding systems like ICD-10 (International Classification of Diseases) and CPT (Current Procedural Terminology) are updated regularly. Invest in an ongoing training program for your coding staff to ensure they know the latest coding guidelines.
- Implement a strong coding compliance program: Establish clear internal protocols for accurate code selection and documentation review. Regular audits can identify potential coding errors and prevent future issues.
- Invest in qualified coding professionals: Hire experienced and certified medical coders who can accurately translate patient encounters into the appropriate codes.
- Utilize clinical documentation improvement (CDI) initiatives: Ensure clear and concise physician documentation accurately reflects the services provided. This facilitates accurate code selection by coders.
Staying Updated with Regulatory Changes:
The healthcare industry is constantly changing, including coding regulations. Here’s how to stay updated:
- Subscribe to industry publications and coding organizations: Stay updated on upcoming coding changes through reliable sources like the American Medical Association (AMA) or the American Academy of Professional Coders (AAPC).
- Attend coding workshops and conferences: Participating in industry events can provide valuable insights into new coding guidelines and best practices.
- Partner with a reliable RCM solution provider: We can help you navigate and ease the complexities of medical coding.
Technology-Assisted Coding Solutions:
ProMantra offers a range of technology solutions designed to streamline and optimize your coding practices:
- Computer-assisted coding (CAC) software: We can help you implement CAC tools that suggest appropriate codes based on patient encounter documentation, improving accuracy and efficiency.
- Automated coding compliance audits: Utilize our automated auditing tools to identify potential coding errors before claim submission, preventing denials and delays.
- Coding education and support: We offer ongoing training and support programs to ensure your coding staff remains up-to-date on the latest coding guidelines and best practices.
By implementing these best practices and leveraging technology-assisted solutions from us, you can optimize your coding processes within the RCM process. This will ensure accurate capture of all billable services, leading to faster reimbursements, maximized revenue, and improved financial health for your healthcare organization.
Critical Way #3: Leverage Technology for Automation and Efficiency Healthcare RCM
In today’s fast-paced healthcare environment, manual processes can become bottlenecks, hindering efficiency and profitability. Fortunately, technology offers a powerful solution: automation. By leveraging innovative tools for automating repetitive tasks within the RCM revenue cycle management process, you can streamline workflows, minimize errors, and free up valuable staff time to deliver focused patient care.
Benefits of Automation in RCM:
Automation offers several compelling advantages for healthcare organizations:
- Increased Efficiency: Automating repetitive tasks like claims submission, eligibility verification, and denials management frees up staff time to deliver a focus on higher-value activities like patient interaction or resolving complex issues.
- Reduced Errors: Manual data entries are prone to errors. Automation reduces and minimizes these errors by ensuring accurate data transfer and reducing human intervention.
- Faster Reimbursements: Automated claim submission and follow-up can significantly expedite the processing time, leading to faster reimbursements and improved cash flow.
- Improved Productivity: Staff can focus on more strategic tasks while automation handles the administrative burden, increasing productivity overall.
Specific Technology Solutions from ProMantra (RCM revenue cycle management):
We offer a comprehensive suite of technology solutions designed to automate and optimize your RCM processes:
- Automated Claims Submission: Our integrated systems electronically submit claims directly to insurance companies, eliminating manual processes and minimizing errors.
- Denial Management Tools: Our advanced software can identify potential denials upfront and guide your team through appeals, maximizing claim recovery opportunities.
- Automated Follow-up and Reporting: Automated systems can handle timely claim follow-up and provide real-time reports on RCM performance, allowing proactive identification and resolution of issues.
- Advanced Data Analytics: Our data analytics tools can identify trends and areas for improvement within your RCM processes, enabling data-driven decision-making for further optimization.
Enhancing Efficiency with End-to-End RCM Revenue Cycle Management:
Our solutions go beyond individual tasks, facilitating a holistic approach to RCM optimization. We promote end-to-end revenue cycle management, where all aspects of the RCM process, from patient registration to payment collection, are seamlessly integrated and automated. This interconnected approach ensures smooth data flow, minimizes errors, and maximizes revenue capture throughout the entire revenue cycle.
Investing in the Future:
By embracing automation and leveraging ProMantra’s innovative technology solutions, you can transform your RCM from a burden to a strategic advantage. Improved efficiency, reduced errors, and faster reimbursements all contribute to a more financially sound and sustainable healthcare organization, allowing you to focus on what matters most – delivering excellent patient care.
Critical Way #4: Prioritize Staff Training and Communication
The success of any RCM system hinges on your most valuable asset – your staff. A well-trained and well-coordinated team can navigate the complexities of RCM efficiently and effectively. Here’s why investing in staff training and communication is crucial.
The Power of a Well-Trained Staff:
- Improved Accuracy and Efficiency: Staff equipped with a thorough understanding of RCM best practices can minimize errors in coding, billing, and claims processing, leading to smoother workflows and reduced denials.
- Enhanced Patient Experience: Knowledgeable staff can answer patient billing questions effectively and navigate the financial aspects of their care more confidently, improving overall patient satisfaction.
- Proactive Problem Solving: A trained team can identify potential RCM issues early on, allowing for proactive solutions before they escalate into more significant problems.
The Importance of Clear Communication:
Effective communication across departments plays a vital role in a seamless RCM process:
- Front-End and Back-End Collaboration: Clear communication between receptionists, billing staff, and coders ensures accurate information flow from patient registration to claims submission.
- Interdepartmental Coordination: Open communication across departments, such as clinical and administrative teams, can prevent delays and ensure everyone is working towards the same goals.
- Improved Patient Engagement: Clear communication with patients about their billing responsibilities and insurance coverage can avoid confusion and build trust.
ProMantra: Your Partner in RCM Training and Support
We understands the importance of a skilled and well-coordinated RCM team. We offer a range of training and support services to empower your staff:
- Comprehensive RCM Training Programs: We provide customized training programs for different staff levels, covering RCM best practices, coding guidelines, and the latest regulations.
- Ongoing Support and Resources: We offers ongoing support and access to industry resources to ensure your staff remains up-to-date and confident in their RCM skills.
- Communication and Collaboration Strategies: We can help you develop strategies to foster clear communication and collaboration between departments, leading to a more cohesive and efficient RCM system.
By prioritizing staff training and communication, you can empower your team to navigate the complexities of RCM and contribute significantly to your organization’s financial health. Partnering with us can equip your staff with the knowledge, resources, and ongoing support they need to excel in RCM.
Critical Way #5: Implement Performance Monitoring and Analytics (Revenue Cycle Optimization)
In the dynamic world of healthcare, continuous monitoring and improvement are essential for a sustainable and efficient RCM system. This is where performance monitoring and data analytics come into play. By tracking key metrics and leveraging data insights, you can identify areas for improvement and make data-driven decisions to optimize your revenue cycle (revenue cycle optimization).
The Power of Measurement:
Effective RCM hinges on the ability to measure performance and identify areas for improvement. Here’s why tracking key RCM metrics is crucial:
- Identify Bottlenecks and Inefficiencies: Metrics like denial rates, claim processing times, and collection rates can reveal bottlenecks and inefficiencies within your RCM process.
- Benchmark Your Performance: Comparing your metrics against industry benchmarks can identify areas where you fall short and opportunities for improvement.
- Track Progress and ROI: By monitoring key metrics over time, you can track the effectiveness of implemented changes and measure the return on investment (ROI) of your RCM optimization efforts.
Key RCM Metrics to Track:
Here are some essential RCM metrics to monitor for effective performance measurement:
- Denial Rate: The percentage of claims denied by insurance companies. A high denial rate indicates potential coding, billing, or insurance verification issues.
- Accounts Receivable (AR) Days: The average days it takes to collect payments after a service is rendered. A high AR day count suggests delays in collecting patient payments.
- Clean Claim Rate: The percentage of claims that are submitted to insurance companies processed without errors. A low clean claim rate indicates potential problems with coding or billing accuracy.
- Collection Rate: The percentage of total charges successfully collected from patients or insurance companies.
Unlocking Insights with Data Analytics: Revenue Cycle Optimization
Data analytics goes beyond simply measuring performance. By analyzing vast amounts of RCM data, you can uncover valuable insights to optimize your revenue cycle:
- Identify root causes of denials: Analyse denial trends to identify patterns and pinpoint specific areas for improvement in coding, billing, or communication with insurance companies.
- Predict patient payment behavior: Leverage data analytics to predict patient payment behavior and identify patients at high risk of non-payment, allowing for proactive collection strategies.
- Resource allocation: Data insights can help you optimize staff scheduling and resource allocation based on patient volume, insurance mix, and service types.
ProMantra: Your Partner in Data-Driven RCM Optimization
We empower you to harness the power of data analytics for revenue cycle optimization. We offer:
- Advanced Data Analytics Tools: We provide sophisticated analytics tools that provide real-time insights into your RCM performance, allowing for proactive decision-making.
- Customizable Reporting Dashboards: Our customizable dashboards deliver clear and concise visualizations of key RCM metrics, enabling you to track progress and identify trends quickly.
- Data-Driven Recommendations: Our team of RCM experts will analyze your data and provide actionable recommendations and suggestions to optimize your revenue cycle based on the insights revealed.
By implementing performance monitoring and leveraging data analytics, you can transform your RCM system from a reactive function to a proactive driver of financial performance. Partnering with us equips you with the tools and expertise to leverage data insights and achieve optimal revenue cycle optimization.
The ProMantra Advantage: Optimizing Your RCM for Success in the US Healthcare Landscape
In today’s competitive US healthcare environment, ensuring a smooth and efficient revenue cycle management (RCM) system is no longer a luxury; it’s a necessity. Partnering with us offers a multitude of benefits that can transform your RCM from a burden to a strategic advantage.
Why Choose ProMantra?
Here’s what sets us apart and positions us as your ideal partner for RCM optimization:
- Comprehensive RCM Solutions: We offer a holistic suite of services encompassing everything from front-end process streamlining to advanced data analytics. Our solutions are tailored and personalized to address the specific needs of US healthcare providers, ensuring a seamless fit within your existing workflows.
- Deep Industry Expertise: Our team comprises experienced RCM professionals with a subtle understanding of the complexities of the US healthcare system, including evolving regulations and coding requirements. This expertise ensures we can provide relevant solutions and guidance for your needs.
- Technology-Driven Approach: We leverage cutting-edge technology solutions to automate tasks, improve accuracy, and empower data-driven decision-making. We stay at the forefront of RCM technology to ensure you have access to the latest advancements.
- Focus on Staff Training and Support: We understand that your staff is the backbone of your RCM system. We offer comprehensive training programs and ongoing support to ensure your team has the latest knowledge and skills to excel in RCM best practices.
- Measurable Results and ROI: We are committed to delivering measurable positive results and a positive return on your investment (ROI). Our performance monitoring and analytics tools enable you to monitor progress and showcase the impact of our RCM solutions on your financial performance.
Partner with Us and Experience the Difference
By partnering with us, you gain a dedicated team of RCM experts who will work collaboratively with you to streamline your processes, improve efficiency, and maximize your revenue capture. We are confident that our solutions can significantly upgrade your financial health and allow you to focus on what matters most – delivering and growing excellent patient care.
The key takeaways are:
- Streamlining RCM processes reduces errors and delays, leading to faster reimbursements.
- Accurate coding and efficient charge capture ensure you capture all billable services.
- Technology automates tasks, improves accuracy, and empowers data-driven decisions.
- Well-trained staff and clear communication are essential for a smooth workflow.
- Data analytics provides insights to identify areas for improvement and optimize your RCM.
By proactively optimizing your revenue cycle management system, you can free up valuable resources, focus on patient care, and ensure the long-term financial health of your healthcare organization. We stand ready to be your trusted partner in achieving RCM excellence. Contact us today, and let’s unlock the full potential of your revenue cycle!
Take the Next Step: Schedule Your Free Consultation!
Are you ready to unlock the full potential of your RCM system? Contact Us today to schedule a free consultation with one of our RCM specialists. We will evaluate your requirements and explore how our comprehensive solutions can enhance your revenue cycle and promote long-term financial success for your healthcare organization.
