A complete guide on Denial Prevention
Did you know that an estimated 10-20% of all healthcare claims submitted in the United States are denied by insurance companies? This translates to billions of dollars lost annually for healthcare providers. Claim denials impact a practice’s bottom line, create significant administrative burdens, and disrupt cash flow.
Effective denial management in healthcare is no longer an option; it’s necessary. This blog post will equip you, the healthcare provider, with the knowledge and strategies to significantly reduce claim denials and optimize your revenue cycle.
What are Claim Denials?
A claim denial occurs when an insurance company refuses to pay for a submitted healthcare service. This can happen for various reasons, including:
- Coding errors: Incorrect or incomplete medical coding can lead to denials if the claim doesn’t accurately reflect the services provided.
- Missing or inadequate documentation: Lack of supporting medical records or justification for medical necessity can also result in denials.
- Authorization issues: Services requiring prior authorization but not obtained before service rendering can be denied.
- Policy exclusions: The service may not be covered under the patient’s insurance plan.
The Financial Consequences of Denials:
Claim denials pose a significant financial burden on healthcare providers. Here’s how:
- Lost Revenue: Denied claims represent lost income for the practice. The sheer volume of denials, even at a rate of 10-20%, can translate to a substantial loss of revenue.
- Increased Administrative Costs: Staff time researching denial reasons, filing appeals, and resubmitting claims adds to administrative expenses.
- Cash Flow Disruption: Denied claims delay reimbursements, impacting a practice’s cash flow and hindering its ability to invest necessary resources and staff.
Beyond the Financials:
The impact of denials extends beyond financial losses. Denied claims can also lead to:
- Patient Frustration: Delays in receiving care due to denied claims can cause frustration for patients.
- Strained Provider-Patient Relationships: When patients are responsible for unexpected costs due to denials, their relationship with the provider can be strained.
In essence, claim denials create a ripple effect that negatively impacts healthcare providers and patients. Implementing effective denial management strategies can significantly mitigate these negative consequences.
How Denials Impact Patient Care
Claim denials aren’t just a financial headache for healthcare providers; they can also hurt patient care. Let’s explore this ripple effect:
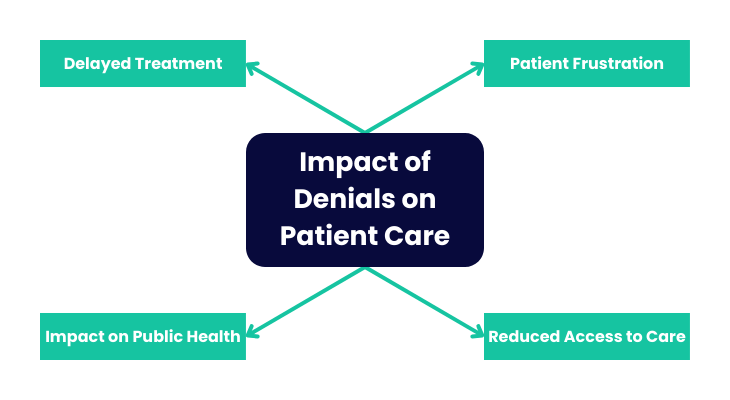
Delayed Treatment:
- When a claim is denied, the patient may be responsible for the cost of the service upfront. This can create a financial barrier, leading to delayed treatment or skipped future appointments.
- Delays in care can worsen a patient’s condition, potentially requiring more intensive and expensive treatment.
Patient Frustration:
- Receiving a bill for a service they thought was covered by insurance can be frustrating and stressful for patients.
- Dealing with denials and appeals can be a time-consuming and confusing, adding to patient frustration.
- This frustration can lead to strained relationships between patients and providers, potentially causing patients to seek care elsewhere.
Reduced Access to Care:
- Repeated denials can discourage patients from seeking necessary care, fearing the potential financial burden.
- This concerns preventive care services, which are crucial for maintaining good health.
Impact on Public Health:
- When patients avoid essential healthcare services due to denials, it can contribute to a decline in overall public health.
By implementing effective denial management strategies, healthcare providers can help ensure timely and affordable patient care access. This not only improves patient satisfaction but also contributes to better health outcomes.
Proactive Denial Prevention for Optimal Revenue Cycle Management
The good news is that claim denials are not inevitable. Healthcare providers can significantly reduce the number of denials they face by adopting a proactive approach to denial prevention. It identifies and addresses potential issues before they lead to claim rejections. This proactive approach offers several benefits:
- Minimized Revenue Loss: Fewer denials translate to fewer lost reimbursements and a healthier bottom line.
- Reduced Administrative Burden: Less time spent managing denials frees up staff resources for other crucial tasks.
- Improved Cash Flow: Timely claim reimbursements ensure a steady cash flow for the practice.
- Enhanced Patient Satisfaction: Avoiding denials minimizes patient frustration and fosters positive patient experiences.
Healthcare providers nationwide face the challenge of minimizing denials and maximizing revenue. Understanding the root causes of denials and implementing effective prevention strategies is crucial for financial stability and patient satisfaction.
The Cost of Claim Denials:
Claim denials are more than a minor inconvenience; they represent a significant financial burden for healthcare providers. Let’s explore the true cost of denials and their impact on practice profitability, operational efficiency, and cash flow.
Financial Impact: A Substantial Loss
- Industry data suggests that insurance companies deny 10-20% of all healthcare claims submitted in the US.
- This translates to billions of dollars lost annually for providers. Even a seemingly small denial rate can significantly impact a practice’s bottom line.
Profitability Under Pressure:
- Denied claims represent lost revenue, directly impacting a practice’s profitability.
- The cumulative effect of these denials can make it challenging for practices to maintain financial stability, especially in today’s competitive healthcare landscape.
Understanding Common Denials in Medical Billing:
Analyzing the reasons behind denials is crucial for developing effective prevention strategies. Some of the most common reasons for claim denials include:
- Coding errors: Incorrect or incomplete medical coding can lead to denials if the claim doesn’t accurately reflect the services provided.
- Missing or inadequate documentation: Lack of supporting medical records or justification for medical necessity can also result in denials.
- Authorization issues: Services requiring prior authorization but not obtained before service rendering can be denied.
- Policy exclusions: The service may not be covered under the patient’s insurance plan.
By understanding these common pitfalls of denial management in healthcare, practices can implement targeted strategies to prevent such rejections and safeguard their revenue.
Operational Impact: Time Consumed, Resources Strained
Managing denials adds a significant administrative burden to healthcare practices. Staff time is dedicated to:
- Researching denial reasons: Understanding the cause of the denial requires staff time to review claim details and payer communications.
- Filing appeals: If a denial is deemed unjust, staff needs to dedicate time to gather supporting documentation and submit a formal appeal.
- Resubmitting claims: Depending on the reason for denial, corrected claims might need to be resubmitted, further adding to the workload.
This time spent managing denials takes away from other crucial tasks like patient care coordination and billing efficiency.
Cash Flow Disruption
Denied claims disrupt a practice’s cash flow, while reimbursements for approved claims form the backbone of that cash flow.
- Delayed payments: Denied claims lead to delayed or even lost reimbursements, creating a cash flow gap.
- Limited resources: Disrupted cash flow can hinder a practice’s ability to invest in necessary equipment, technology, and staff resources, impacting its long-term growth and competitiveness.
By implementing effective denial management strategies, healthcare providers can streamline their revenue cycle, optimize cash flow, and ensure the financial sustainability of their practice.
Strategy 1:
Streamline Coding and Documentation
Accurate coding and comprehensive documentation are the cornerstones of effective denial prevention. Here’s how you can ensure your practice lays a solid foundation for clean claim submissions:
Focus on Accurate Coding:
Invest in ongoing training for your coding staff to stay up-to-date on the latest coding guidelines (ICD-10, CPT, HCPCS). Utilize robust coding software with built-in edits and compliance checks to minimize errors. Implement regular internal audits to identify and rectify any coding inconsistencies.
Complete and Up-to-date Documentation:
Physicians play a crucial role in maintaining detailed, accurate, and timely medical records. Documentation should justify medical necessity for all services rendered, including diagnoses, procedures, and supporting findings. Ensure timely completion of charts to avoid delays in claim submission.
Specificity is Key:
Don’t settle for generic codes! Strive for the highest level of specificity when selecting codes. Capture all relevant service details, including diagnoses, procedures, modifiers, and laterality. This level of detail ensures your claims accurately reflect the complexity of the care delivered.
By prioritizing accurate coding and comprehensive documentation, you significantly reduce the risk of denials due to missing information, coding errors, or inadequate justification for medical necessity. This improves your chances of first-pass claim approval and strengthens your appeals if denials do occur.
Strategy 2:
Master Prior Authorizations – Avoid Delays and Denials
Prior authorizations, a growing trend in healthcare, can significantly impact claim processing times. Understanding these requirements and implementing a streamlined management system is crucial for denial prevention.
Understanding Prior Authorization Requirements:
Prior authorization is when a healthcare provider obtains approval from a patient’s insurance company before rendering specific services. Common examples include certain procedures, medications, or diagnostic tests. Knowing which services require prior authorization and understanding payer-specific guidelines are vital for avoiding denials.
Developing a System for Prior Authorization Management:
Embrace technology! Utilize electronic health records (EHRs) to submit authorization requests electronically, streamlining the process and reducing potential errors. Develop strong communication channels with payer representatives to clarify any ambiguities and ensure timely approvals.
Proactive Approach is Key:
Be sure to arrive on the day of service! Proactively check for prior authorization requirements before the planned visit or procedure. This allows ample time to secure approvals and avoid delays or denials due to missing authorization.
By mastering prior authorizations, you can ensure a smoother claims journey, minimize delays, and significantly reduce the risk of denials related to missing approvals.
Strategy 3:
Leverage Technology for Efficiency – Empowering Denial Management in Healthcare
In today’s digital age, technology offers powerful tools to optimize denial management in healthcare. Let’s explore how leveraging technology can significantly improve your denial prevention efforts.
Benefits of Denial Management Software:
Investing in denial management software can be a game-changer. This software can analyze denied claims, identify recurring trends, and pinpoint the root causes. This valuable insight allows you to focus your prevention efforts on areas with the highest impact. Denial management software can also streamline the appeals process, saving you valuable time and resources.
Automating Claim Submission:
Embrace automation! Utilizing technology for automated claim submission can significantly reduce errors and expedite claim processing times. Computerized systems can perform basic edits and checks, catching potential coding mistakes before submission and minimizing the risk of denials due to technical errors.
Data Analytics for Insights:
Data is power! Denial management software often comes equipped with powerful data analytics tools. These tools can provide valuable insights into denial patterns, such as specific procedures or diagnoses frequently denied by certain payers. By analyzing this data, you can identify areas for improvement and tailor your coding and documentation practices to address these recurring issues.
By effectively leveraging technology, healthcare providers can streamline workflows, minimize errors, and gain valuable insights to proactively address potential denial risks. Remember, technology is a powerful tool in your denial prevention arsenal.
Strategy 4:
Stay Informed on Payer Policies – Navigate the Ever-Changing Landscape
The healthcare landscape is constantly evolving, and payer policies are no exception. Staying informed about changes to coverage rules and reimbursement requirements is crucial for preventing denials.
Understanding Payer Policies:
Understanding the specific rules and regulations of each payer you work with is vital. Payer policies can dictate coverage for particular services, coding requirements, and documentation expectations. A lack of awareness regarding these policies can lead to denials due to services not being covered or claims not meeting specific formatting criteria.
Payer Websites and Resources:
Feel free to leverage the resources available! Most payers maintain websites with detailed information about their policies, coverage guidelines, and coding requirements. Regularly checking these websites and subscribing to their updates ensures you stay abreast of any policy modifications that might impact claim reimbursement.
Building Relationships with Payer Representatives:
Developing positive relationships with payer representatives can be a valuable asset. These representatives can clarify complex or unclear policies, answer specific questions about claim submissions, and offer guidance during appeals.
By staying informed about payer policies and fostering positive relationships with payer representatives, you can confidently navigate the ever-changing healthcare landscape, minimizing the risk of denials due to policy oversights.
Strategy 5:
Invest in Staff Training and Development – Empowering Your Denial Management Team
Your staff is your frontline defense against denials. By investing in their knowledge and skills, you empower them to become proactive champions of denial prevention.
Comprehensive Training Programs:
A knowledgeable staff is a powerful asset. Implement ongoing training programs for coders, billers, and other revenue cycle staff. These programs should keep them updated on the latest coding standards (ICD-10, CPT, HCPCS), payer policies, and best practices for denial prevention. Consider incorporating training on specific denial trends and common pitfalls to equip your team with the knowledge to identify and address potential issues before they lead to denials.
Communication and Collaboration:
Foster a culture of open communication and collaboration within your practice. Encourage staff to communicate any uncertainties regarding coding, documentation, or payer requirements. Early identification and rectification of errors in the billing process can significantly reduce the risk of denials later on.
Investing in Staff Knowledge – A Smart Choice:
Investing in staff training is not an expense but an investment in your practice’s financial health. A well-trained staff with the latest knowledge and best practices can significantly reduce claim denials, improve revenue cycle efficiency, and contribute to your practice’s overall profitability. Consider exploring certifications for your coding and billing staff, such as the Certified Professional Coder (CPC) or Certified Medical Billing Specialist (CMBS). Additionally, some practices might benefit from hiring a dedicated denial management specialist to oversee the denial management process and ensure best practices are consistently followed.
Empowering your staff through ongoing training and fostering a collaborative environment creates a team dedicated to minimizing denials and optimizing your revenue cycle.
The Appeals Process: Fighting for Reimbursement
While denial prevention is the key strategy, there will be instances where claims are denied. Don’t despair! Not all denials are final. You can appeal the decision if you believe a claim was wrongly denied. However, navigating the appeals process can be complex. Here’s what you need to know:
Not All Denials are Final:
Understanding the reason for denial is crucial. Common denials in medical billing often stem from coding errors, missing information, or lack of justification for medical necessity. If you believe the denial is due to a mistake or oversight, you can successfully appeal the decision with proper documentation.
Understanding Appeal Timeframes:
Time is of the essence! Each payer has specific deadlines for submitting appeals. These deadlines can ensure your appeal is not automatically denied. Carefully review the remittance advice accompanying the denied claim. This document will typically outline the specific reason for denial and the timeframe for appeal submission.
Crafting a Strong Appeal Argument:
A well-constructed appeal argument is essential for increasing your chances of success. Here are some key elements:
- Clearly state the reason for the appeal: Briefly explain why you believe the claim was wrongly denied. Reference the specific denial code and the reason provided by the payer.
- Provide supporting documentation: This might include medical records, coding references, peer-reviewed articles supporting the medical necessity of the service, or any additional information that strengthens your case.
- Maintain a professional tone: Be clear, concise, and professional. Avoid accusatory language or emotional pleas.
- Meet all deadlines: Ensure you submit your appeal within the timeframe specified by the payer.
Consider Outsourcing Appeals:
For complex denials, particularly those involving large sums or intricate regulations, consider outsourcing the appeals process to experienced professionals. These professionals, often referred to as denial management specialists, have the expertise and resources to navigate the intricacies of the appeals process and significantly improve your chances of a successful outcome.
Remember, the appeals process can be time-consuming and require meticulous attention to detail. By understanding your options, gathering the necessary documentation, and crafting a solid appeal argument, you can fight for the reimbursement you deserve for the services you provide.
Proactive Denial Management: A Continuous Process for Optimal Revenue Cycle Health
Denial prevention isn’t a one-time fix; it’s an ongoing commitment to optimizing your revenue cycle. Shifting from a reactive approach (simply reacting to denials) to a proactive one (focusing on prevention) is crucial in minimizing denials and maximizing reimbursements.
Regular Denial Review:
Schedule regular dental reviews, whether weekly or monthly, to analyze denied claims. This analysis, ideally led by a denial management specialist or a dedicated team member, should involve:
- Identifying recurring denial trends: Are there specific codes, procedures, or payers with a high denial rate? Understanding these patterns allows you to tailor your prevention strategies to address the most impactful issues.
- Root cause analysis: Dig deeper to understand the reasons behind denials. Is it a coding error, missing documentation, or a lack of clarity in payer policies? Addressing the root cause prevents similar denials from occurring in the future.
Building a Denial Prevention Culture:
Effective denial management requires a team effort. Here’s how to foster a culture of denial prevention within your practice:
- Staff Education: Invest in ongoing training programs for all staff involved in the revenue cycle – from front-desk personnel to physicians. Educating everyone on best practices for coding, documentation, and communication with payers empowers them to identify and address potential issues before they lead to denials.
- Open Communication: Encourage open communication between staff regarding any uncertainties or challenges they encounter throughout the claim submission process. Early identification and rectification of errors significantly reduce the risk of denials later on.
- Performance Tracking and Incentives: Consider implementing performance metrics focused on denial rates and successful claim submissions. This can incentivize staff to prioritize clean claim submissions and contribute to a culture of denial prevention.
By adopting a proactive approach, regularly analyzing denials, and fostering a collaborative environment, you can create a sustainable system for minimizing denials and ensuring the financial health of your practice. Remember, even minor improvements in denial rates can translate to significant economic gains over time.
Taking Control of Your Revenue Cycle – The Power of Denial Prevention
Claim denials significantly burden healthcare providers, impacting everything from profitability to cash flow and patient satisfaction. By implementing the denial prevention strategies outlined in this blog post, you can take control of your revenue cycle and significantly reduce the risk of denials.
The Value of Denial Management:
Effective denial prevention offers a multitude of benefits for healthcare providers:
- Increased Revenue: Fewer denials translate to more reimbursements and a healthier bottom line.
- Improved Efficiency: Reduced time spent managing denials frees up staff resources for other crucial tasks.
- Enhanced Cash Flow: Timely claim reimbursements ensure a steady cash flow for the practice.
- Stronger Patient Relationships: Minimized denials reduce patient frustration and contribute to a better overall patient experience.
Call to Action: Empower Your Practice
Don’t let denials erode your practice’s financial health! Act today to implement these denial prevention strategies and optimize your revenue cycle.
We understand that navigating the complexities of denial management can be challenging. ProMantra offers a range of denial management services for those seeking additional support to help healthcare providers significantly reduce denials and maximize revenue recovery.
ProMantra’s Expertise: Your Partner in Denial Prevention
ProMantra has a proven track record of helping healthcare providers nationwide achieve significant improvements in their denial rates. Our denial management specialists have the experience and expertise to guide you through every step of the denial prevention process, from identifying root causes to crafting successful appeals.
Schedule a Free Consultation:
Take the first step towards a healthier revenue cycle. Contact ProMantra today for a free consultation with our denial management experts. Discuss your specific challenges and explore how ProMantra can help your practice thrive.
By prioritizing denial prevention and embracing a proactive approach, you can ensure your practice receives the reimbursements it deserves for the high-quality care you provide.