
Healthcare is indeed the most complex landscape to navigate. However one of the most pivotal aspects of healthcare operations is Healthcare is complex, and Revenue Cycle Management (RCM) plays a vital role in maintaining financial stability. RCM covers everything from scheduling appointments to processing final bill payments, streamlining operations, and reducing administrative costs.
Prior Authorization (PA) is one of the most challenging parts of RCM. An AMA survey shows that physicians handle an average of 45 PA requests per week, spending nearly two business days on them. About 35% of physicians have staff dedicated to handling PAs, with 88% describing the process as a heavy burden. Over the last five years, PA requirements have grown, adding to the workload.
Outsourcing PA has become a strategic solution to these challenges. In this blog, we’ll discuss why outsourcing prior authorization service is key to improving the financial health of healthcare providers.
Outsourcing prior authorization services involves efficiently managing authorization tasks through third-party providers, which enhances operational efficiency and accelerates patient access to essential healthcare treatments and diagnostics. These third-party services act as intermediaries with payers, such as insurance companies or Medicaid, handling patient data collection for authorizations to ensure a centralized, error-minimized process. They manage complete pre-authorization processes, follow up on additional information needs, and handle appeals for denied requests. This approach can significantly save your practice time and money.
Here are some key benefits that come from outsourcing prior authorization
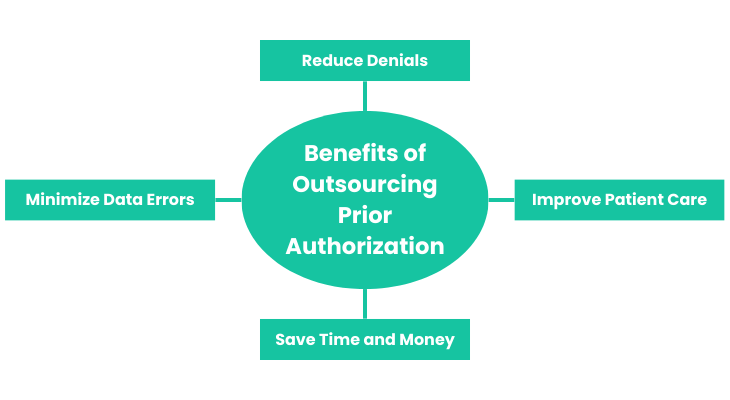
Outsourcing prior authorization is one of the best decisions a healthcare organization can ever make. It is quite simple: the healthcare providers, when handling PA in-house, lack the required staffing and the latest knowledge on compliance and policies. Moreover, they regulate the process manually, which takes a longer time.
This, in turn, results in longer waiting periods and high denial rates. This is not doing any good to them as they are losing patents and revenue.
However by outsourcing PA, healthcare organizations can leverage the expertise of dedicated professionals who are well-versed in the latest regulatory requirements and payer policies.
These experts use advanced technologies and automated systems to streamline the PA process, ensuring that all necessary documentation is accurate and complete. This reduces the chances of errors and increases the chances of approval.
The costs associated with in-house prior authorization management can be quite a lot for healthcare providers.
Some studies suggest that this process can cost between $80 and $100 per request. Outsourcing prior authorization services, such as those offered by ProMantra, can significantly reduce these costs, allowing providers to redirect resources to other critical areas.
Outsourcing PA can also save healthcare providers significant time and money. Managing PA in-house requires substantial administrative resources, including hiring and training staff, maintaining up-to-date knowledge of payer requirements, and handling the time-consuming tasks associated with the PA process.
Outsourcing these tasks allows healthcare providers to reallocate their resources more efficiently.
It is from the reports that a clinic that outsourced its Prior Authorization process reported saving an average of 20 hours per week, which could then be utilized in patient care and other critical tasks.
Financially, outsourcing PA can lead to substantial cost savings. Medical practices can avoid the costs associated with denied claims and rework by reducing the need for in-house staff and lowering denial rates.
Additionally, outsourcing partners often operate on a performance-based model, meaning their fees are tied to the success of the PA process, further incentivizing efficiency and accuracy.
Inaccurate data is an important reason behind claim denials and also complicates the issues even further. However, outsourcing partners reduce data errors as they have specialized staff who are trained to work on data accurately.
These partners typically use advanced EHR systems and have automated workflows. The automation lets them ensure the work is done accurately and quickly. These systems can find faults in data and can flag the issues. They can also find the miss in the data so that they do not miss out on anything. This ensures the data accuracy.
Outsourcing PA can positively impact patient care and clinical outcomes. When healthcare providers are bogged down by administrative tasks, they have less time to focus on their primary responsibility: patient care. By outsourcing PA, providers can free up valuable time and resources, allowing them to devote more attention to their patients.
Improved PA processes also lead to quicker approvals for necessary treatments and medications, reducing patient care delays. This can be particularly important for patients requiring urgent or specialized treatments. Additionally, outsourcing can enhance patient satisfaction by reducing the frustration and uncertainty associated with PA delays and denials.
Effective PA management involves several key components that streamline the process, improve patient care, and enhance collaboration between providers and payers.
One of the major components of PA management is accurate and comprehensive patient records. Aspects like medical history, patient information, and ongoing medications together constitute an accurate patient record. These records when managed by EHR can be worked upon easily.
Pre-approved authorizations can significantly reduce the administrative burden on providers and improve the overall PA process. These pre-approvals can be based on standardized criteria, such as evidence-based review guidelines, to ensure consistency and efficiency. Documentation requirements should be clear and transparent, and providers should be notified of any changes to the PA process.
So who is all this about? Patient. The patient is the key component of the PA process. The patient’s engagement in a way where he communicates about his condition, his details, and the financial obligations aids in the process to a great extent.
Emerging technologies, such as electronic prior authorization (ePA), are transforming the PA process by reducing administrative burdens and improving efficiency.
These ePA solutions automate the PA process and enable a secure and electronic transmission of patient information, which significantly reduces the time spent on PA reviews.
Prior authorization (PA) is a crucial component of managed care pharmacy, ensuring that patients receive appropriate and timely access to medications and treatments. However, the process is often plagued by inefficiencies, inconsistencies, and evolving rules, making it challenging for providers and payers to navigate. In this article, we will discuss the common challenges in PA and strategies for overcoming them.

One of the primary challenges in PA is addressing the diverse and complex requirements of different payers. Each payer has its own unique set of rules, guidelines, and criteria for authorizing treatments, which can be overwhelming for providers.
To overcome this challenge, providers must stay up-to-date with the latest payer requirements and maintain detailed knowledge of each payer’s specific needs.
This may involve regularly reviewing payer policies, attending industry events, and networking with peers to stay informed about the latest developments.
Moreover, providers should consider implementing a centralized PA management system that can streamline the process by consolidating payer requirements and automating the submission of PA requests.
This can help reduce the administrative burden and ensure that providers are submitting accurate and complete information to each payer.
Another significant challenge is the inconsistent workflows between payers and providers. Inefficient workflows can lead to delays, errors, and frustration for both payers and providers.
To get these workflows running smoothly, providers should focus on implementing electronic prior authorization (ePA) solutions that automate the PA process which will ensure seamless communication with payers.
ePA solutions can significantly reduce the time and effort required to submit and track PA requests, as they often include features such as real-time eligibility checks, automated data entry, and electronic submission of supporting documentation.
By harnessing the power of ePA, providers can improve the efficiency of their PA management processes and enhance collaboration with payers.
The rules and regulations of insurance companies are continuously evolving. This content update makes it a mandate for providers to stay up to date with the policies and the guidelines of the payers.
This may involve subscribing to industry publications, attending webinars or workshops, or engaging with payer representatives to stay informed about the latest developments.
The providers should also consider implementing a robust compliance management system that can help them track and respond to changes in payer rules and regulations.
This can include features such as automated alerts, policy updates, and compliance reporting to ensure that the organization remains up-to-date and compliant.
Effective PA management requires skilled personnel who can navigate the complex process efficiently.
Providers should invest in training and development programs to ensure that their staff are equipped to handle the demands of PA management.
This may include providing ongoing education on payer requirements, PA submission best practices, and strategies for managing denials and appeals.
Automation has become a part of almost all domains and workflows. Automation in PA authorization can significantly improve the PA process and can enhance the overall practice productivity and revenue.
Automation significantly speeds up the PA process by eliminating manual workflows and reducing the need for manual data entry.
Electronic prior authorization (ePA) solutions can automate the submission of PA requests, reducing the time spent on PA reviews and improving the overall efficiency of the process. This can lead to faster patient access to care and improved patient outcomes.
It reduces the administrative workload associated with PA by automating routine tasks such as data entry, eligibility checks, and submission of supporting documentation.
This can help reduce the chances of medical errors and improve the overall quality of care. Automation also helps to reduce the administrative burden on staff, freeing them up to focus on more value-added tasks.
Automation can provide real-time data insights into the PA process, enabling providers to track the status of PA requests and identify areas for improvement.
This can help improve first-submission success rates by ensuring that all necessary information is captured and transmitted accurately.
Real-time data insights can also help providers identify and address potential issues before they become major problems.
Automation enhances overall practice productivity and revenue by reducing the administrative burden on staff and improving the efficiency of the PA process.
By automating routine tasks and reducing the need for manual data entry, providers can reallocate staff to more value-added tasks, improving overall practice productivity and revenue.
Outsourcing PA management to a reliable partner can significantly improve the efficiency and effectiveness of the process. But how would you choose from so many of them? Well, we have jotted down some key considerations.
Here are some key considerations and questions to ask potential PA management vendors to ensure a successful partnership.
Outsourcing prior authorization can improve efficiency, but it’s important to avoid common mistakes. Here are key pitfalls healthcare providers should watch out for when choosing a partner:
One of the most critical decisions in outsourcing prior authorization is selecting the right provider. Not all providers have the same level of expertise or experience, and the wrong choice can lead to inefficiencies, errors, and higher costs. Healthcare providers should carefully vet potential partners, considering their industry experience, track record, and client reviews. It’s vital to choose a partner who understands your practice’s needs and consistently delivers reliable results.
Clear communication between healthcare providers and outsourcing partners is essential for successful prior authorization. Without transparency, the process can suffer from delays, errors, and misunderstandings. Providers should establish clear communication channels and set expectations with their partner. Regular updates, open dialogue, and transparent reporting are key to ensuring smooth operations and addressing issues promptly.
Outsourcing prior authorization means sharing sensitive patient data. It’s crucial to ensure the provider follows strict compliance and security standards, including those under HIPAA. Providers must confirm that the partner has strong data protection measures and complies with all regulations. Failing to do so can lead to data breaches, legal issues, and reputational damage.
Each healthcare practice has unique needs. A one-size-fits-all approach to prior authorization won’t work. It’s important to choose a provider that offers custom solutions tailored to your practice. This includes understanding the services needing authorization, the insurance plans involved, and your workflow. Customization ensures the provider integrates well with your operations and delivers optimal results.
Even after outsourcing, healthcare providers should monitor the performance of their partner. Key performance indicators (KPIs) like approval rates, turnaround times, and denial frequencies must be reviewed regularly. Monitoring these metrics helps identify issues early and allows for corrective actions. By maintaining oversight, providers can ensure the partnership meets expectations and delivers the desired outcomes.
Key Consideration:
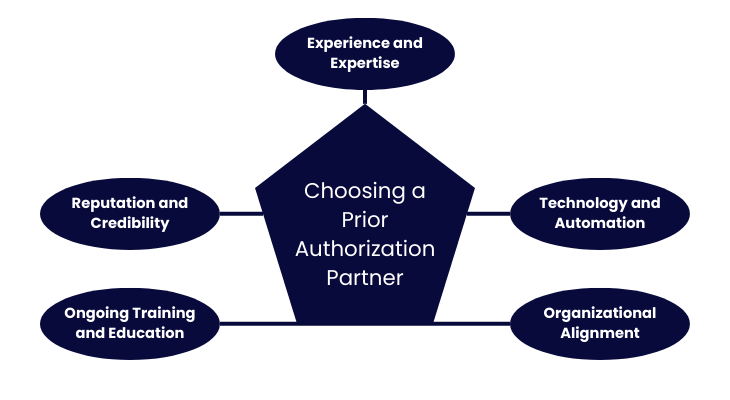
Make sure that the outsourcing partner has decent experience in managing PA processes and a deep understanding of the healthcare industry. Handling complex PA requirements and ensuring compliance with regulatory standards should not be a difficult task for them.
The partner should invest in the latest advancements in technology, such as electronic prior authorization (ePA), to streamline the PA process and reduce administrative burdens.
Any outsourcing partner who shares a similar mission, culture, and values with your organization is the one for you. They should be able to perform the work themselves and not subcontract to other organizations.
The partner should provide ongoing training and education to their staff to ensure they are current on the latest guidelines, rules, and practice standards. This helps maintain high accuracy rates and minimizes denials.
Verify the partner’s reputation by checking references, asking for case studies, and ensuring they have worked with organizations of similar size and complexity.
Prior authorization (PA) is a crucial component of healthcare, ensuring that patients receive appropriate and timely access to medications and treatments.
However, the manual process of PA can be time-consuming, labor-intensive, and prone to errors. Outsourcing PA management to a reliable partner like ProMantra can significantly improve the efficiency and effectiveness of the process.
Key Benefits of Outsourcing Prior Authorization Services
Reach out to us today to learn more about how ProMantra can help you achieve industry-leading standards and key performance indicators.
Our dedicated team is ready to help you navigate the complexities of PA management and ensure that your healthcare organization thrives in a competitive market
Reference: AMA