Strong and efficient revenue cycle management (RCM) is crucial to the financial and operational well-being of every healthcare organization.
RCM is the lifeblood of financial health for healthcare organizations and guarantees that every dollar earned is captured and collected on time.
We at Promantra recognize this, and have, over the years, fine-tuned our RCM services to ensure we ace all our KPIs, and that our clients enjoy a healthy, stress-free cash flow.
Let’s take a quick look at how Promantra has been leading RCM KPIs, making us a preferred RCM provider for healthcare organizations.
Revenue Cycle Management (RCM) and Its Importance in Healthcare
Let us have a look at what importance Revenue Cycle Management holds in healthcare and why can’t it be overlooked at any cost:
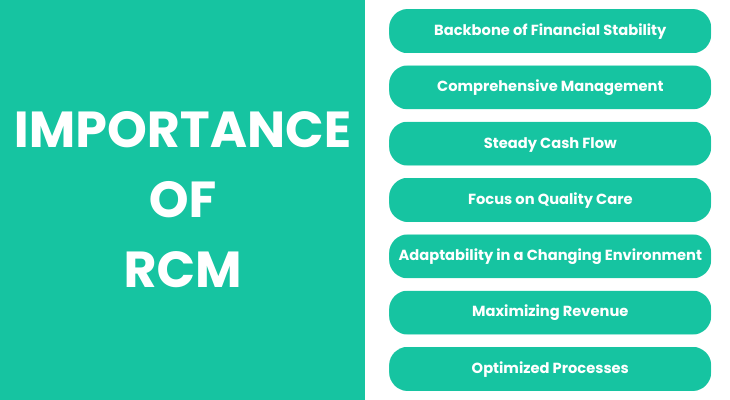
- Backbone of Financial Stability: RCM is crucial in the financial management of healthcare organizations since it determines the flow of revenues.
- Comprehensive Management: RCM encompasses the process of scheduling appointments, the registration of patients, to the payment of medical bills.
- Steady Cash Flow: Good RCM makes certain that the healthcare providers receive constant cash inflows and reduces the chances of claim denials.
- Focus on Quality Care: When RCM is done correctly, the healthcare providers can concentrate on giving out quality services without worrying about the bill.
- Adaptability in a Changing Environment: This is especially important in a healthcare setting where there are constant changes in regulation as well as billing challenges.
- Maximizing Revenue: RCM is a core component in the optimization of revenues, which is associated with patients’ satisfaction and organizational outcomes.
- Optimized Processes: Healthcare providers can also enhance billing, coding, and claims to decrease mistakes and expenses.
An Introduction to Promantra
Promantra has established itself as a Revenue Cycle Management (RCM) company that delivers outstanding performance to healthcare providers.
Being aware of the industry’s problems, Promantra’s approach to RCM is based on the principles of professionalism and constant development.
The management of the company has adopted KPIs, which makes it possible to have a check on every aspect of the revenue cycle.
From days in AR to denial rates, Promantra has set new benchmarks with its data-driven approach.
Their focus on delivering bespoke solutions that address each client’s specific requirements is a testament to their passion for assisting healthcare organizations in realizing their financial potential.
It is not just about the numbers. It is about helping Promantra continue to be a leading light in RCM and supporting healthcare providers to succeed in a more challenging world. By doing so, they can focus on delivering the best possible patient care without worrying about the financial side.
Key KPIs and Promantra’s Best Practices
For any practice to deliver great results in RCM, monitoring and managing scores of KPIs are mandatory.
Promantra not only tracks these critical key performance indicators but also practices what in its view is the best strategy.
Here is a list of the major RCM indicators and how the best practices of Promantra help to increase these figures.
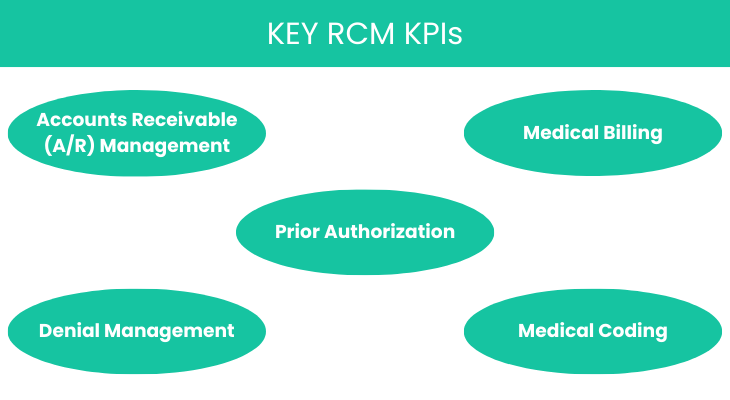
Prior Authorization
Before looking at the special role of prior authorization let’s discuss the situation in the broad context of healthcare.
When done inappropriately, the process may cause problems such as delays and financial crunch.
Significance in RCM: How Prior Authorization Impacts the Revenue Cycle
Prior authorization is a critical component of the revenue cycle in healthcare. It involves obtaining approval from insurance providers before providing specific treatments or services.
This step is essential for ensuring that services are covered and reimbursed, but it can also be a significant source of delays and administrative burdens.
When not managed efficiently, prior authorization can lead to claim denials, delayed payments, and, ultimately, a disruption in cash flow.
For healthcare providers, managing prior authorization effectively is crucial for maintaining a smooth revenue cycle and avoiding financial setbacks.
Promantra’s Expertise: Streamlining the Authorization Process to Reduce Delays and Denials
Promantra excels in streamlining the prior authorization process, leveraging advanced technology and experienced professionals to ensure that authorizations are obtained quickly and accurately.
Automating much of the authorization workflow and implementing rigorous checks enables Promantra to reduce the likelihood of delays and denials.
Their expertise in navigating complex payer requirements allows them to minimize errors and ensure all necessary documentation is provided upfront.
This proactive approach speeds up the authorization process and increases the approval rate, ensuring healthcare providers can deliver care without financial uncertainty.
Efficiency Gains: Demonstrating Improved Turnaround Times and Reduced Administrative Burdens
Promantra’s focus on efficiency translates into significant gains for its clients. Reducing the time required to secure prior authorizations helps Promantra to let healthcare providers improve their overall turnaround times, enabling faster service delivery and billing.
Automating key parts of the process alleviates the administrative burden on healthcare staff, allowing them to focus on patient care rather than paperwork.
These efficiency gains result in a more streamlined revenue cycle, fewer disruptions, and a more predictable cash flow.
Accounts Receivable (A/R) Management
Effective management of Accounts Receivable (A/R) is vital for maintaining the financial health of any healthcare organization.
Providers can avoid cash flow issues and continue delivering high-quality care by ensuring that payments are collected promptly.
Why A/R Matters: The Role of A/R in Cash Flow and Financial Stability
Accounts Receivable (A/R) management is a cornerstone of financial stability for healthcare organizations.
A/R represents the money owed to a healthcare provider for services rendered, and effective management of these receivables is crucial for maintaining a steady cash flow.
The longer receivables remain unpaid, the greater the strain on a provider’s financial resources. Efficient A/R management ensures that payments are collected promptly, reducing the risk of financial shortfalls and enabling healthcare providers to meet operational expenses and invest in quality care.
Promantra’s Strategies
Promantra uses several best practices to manage A/R, including the day’s receivables outstanding, collection speed, and handling of any exceptions.
Some of the strategies they use are follow-ups with the payers, proper and timely billing, and data analysis to determine issues that may likely cause major concerns.
Through the above strategies, Promantra assists the healthcare providers to minimize their A/R days hence enhancing the collection period and cash flow.
Impact on Financial Health: Case Studies Showing Improvements in A/R Metrics
The impact of Promantra’s A/R management strategies is best demonstrated through their clients’ success stories.
Case studies reveal significant improvements in key A/R metrics, such as reduced A/R days and increased collection rates.
For example, one client saw a 15% reduction in A/R days within just a few months of partnering with Promantra, resulting in enhanced financial stability and greater operational flexibility.
These results underscore Promantra’s ability to positively influence the economic health of healthcare providers through expert A/R management.
Medical Billing
Medical billing is pivotal in Revenue Cycle Management (RCM), acting as the engine that drives a healthcare organization’s revenue.
The accuracy and efficiency of this process directly impact financial outcomes, making it a critical component of RCM.
The Core of RCM: How Accurate and Efficient Billing Drives Revenue
Accurate and efficient billing is fundamental to maximizing revenue for healthcare providers. It ensures that claims submitted to insurers are correct and complete, reducing the likelihood of denials and speeding up payments.
A streamlined billing process accelerates cash flow and minimizes administrative overhead, allowing healthcare providers to focus on delivering quality care.
With accuracy in billing, healthcare organizations can avoid significant revenue losses due to denied or delayed claims.
Promantra’s Billing Process: Ensuring Accuracy and Compliance
Promantra’s approach to medical billing is rooted in precision and compliance. Leveraging advanced technology and a team of skilled professionals, Promantra ensures that every claim is meticulously prepared and submitted in adherence to industry regulations.
This process improves billing accuracy and enhances compliance with payer requirements, reducing the risk of penalties and denials.
The commitment of Promantra to continuously improve and do rigorous quality checks ensures its clients experience fewer billing errors and increased financial stability.
Performance Indicators: Success Stories of Increased Billing Accuracy and Reduced Errors
Significant improvements in key client performance indicators indicate Promantra’s medical billing success.
Case studies show a marked increase in billing accuracy, resulting in faster payments and reduced billing errors.
These improvements translate into better cash flow management and a stronger financial position for healthcare organizations.
Denial Management
Denial management is a critical component of Revenue Cycle Management (RCM), directly impacting the financial health and cash flow of healthcare providers.
Effective denial management involves not just addressing denied claims but understanding the underlying patterns that lead to these rejections.
Promantra stands out in this area with its proactive approach to managing denied claims. Their team meticulously analyzes denial patterns to pinpoint the reasons behind claim rejections and takes corrective actions to prevent similar issues in the future.
They are dedicated to recovering lost revenue, going the extra mile to ensure that healthcare providers receive the payments they are rightfully owed.
This approach not only strengthens cash flow but also contributes to the overall financial stability of the organization.
Medical Coding
Medical coding is one of the most important components of the claims processing cycle and can be considered as the foundation for proper billing and timely reimbursement.
Appropriate coding means that all services delivered are coded appropriately and thus reduces the chances of denied claims, and shortens the time taken to be reimbursed.
This is a careful approach that is necessary for healthcare institutions that wish to have a good financial standing and not to experience any form of delay that may affect the cash flow.
Promantra has successfully ruled in this area, with its coding specialists being up to date with the current coding rules and regulations.
Their expertise not only minimizes the occurrence of coding mistakes but also helps in getting reimbursement at a faster pace, which in turn helps in the financial sustainability of the healthcare organizations.
Summing Up
Promantra’s Revenue Cycle Management (RCM) expertise sets a new standard for excellence in healthcare financial services.
Focusing on critical areas such as prior authorization, accounts receivable management, and medical billing, Promantra helps healthcare organizations streamline processes, reduce administrative burdens, and enhance financial stability.
With a proven track record of success, Promantra is not just a service provider but a strategic partner committed to driving growth and efficiency in the healthcare sector.
Ready to improve your Revenue Cycle Management? Partner with Promantra to optimize your financial processes and achieve measurable results.
Contact us today to learn how our tailored solutions can transform your RCM operations and help your organization thrive in the healthcare landscape.




