We all agree that Prior Authorization has emerged as a critical process that significantly impacts patient care and financial outcomes for healthcare providers. However, the complexities and administrative burdens associated with prior authorization can lead to inefficiencies and financial strain. Let’s explore the benefits of offshoring prior authorization services to top companies in the industry. By leveraging the expertise and resources of these specialized providers, healthcare organizations can transform their operations, optimize cash flow, and enhance patient care.
The Importance of Prior Authorization Services:
Prior authorization has become increasingly vital in the healthcare industry, acting as a gatekeeper for patients seeking certain treatments or procedures. This process ensures that insurance companies approve the medical necessity and coverage of requested services, safeguarding patient care and financial stability. However, managing prior authorization internally can be challenging for healthcare organizations.
The extensive administrative tasks, complex workflows, and evolving regulations can lead to inefficiencies and increased costs. As a result, outsourcing prior authorization services to top companies in the field has emerged as a strategic solution to optimize operations, enhance revenue cycle management, and deliver improved patient outcomes.
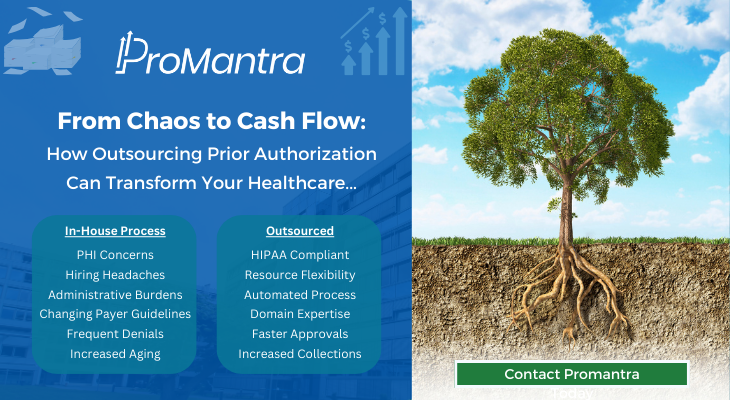
The Challenges of In-house Prior Authorization:
The manual nature of the Prior-Auth process, involving extensive paperwork, phone calls, and follow-ups, can be time-consuming and prone to errors. Inefficient workflows and limited resources can lead to delays in obtaining approvals, resulting in delayed patient care and potential revenue loss. Additionally, the ever-changing landscape of insurance requirements and regulations further complicates the in-house management of prior authorization.
With increasing denial rates, healthcare organizations bear the burden of appeals and resubmissions, impacting both financial stability and patient satisfaction. Outsourcing prior authorization to experienced companies like Promantra alleviates these challenges, enabling providers to focus on core operations while ensuring a streamlined, accurate, and timely authorization process.
Outsourcing prior authorization services to top Prior Authorization companies like Promantra brings a multitude of benefits to healthcare organizations. Promantra possess extensive knowledge and expertise in navigating the complex landscape of insurance requirements, coding, and documentation. By leveraging our experience, healthcare organizations can streamline their prior authorization processes, reduce administrative burdens, and improve overall efficiency.
Outsourcing also enables access to advanced technology and automation tools, eliminating manual tasks and reducing errors. This leads to faster turnaround times, increased approval rates, and enhanced cash flow. Furthermore, outsourcing allows healthcare providers to tap into a network of resources, including dedicated teams of experts, robust reporting capabilities, and ongoing support. By partnering with the best prior authorization companies, healthcare organizations can transform their operations, optimize revenue cycle management, and ultimately deliver better patient care.
Choosing the Best Prior Authorization Company:
Selecting the right outsourcing partner for prior authorization is crucial to ensure a successful transition. Healthcare organizations should consider several factors when making this decision. First and foremost is the prior authorization company’s industry experience and track record of success. A reputable company like Promantra with a proven history of delivering results will instil confidence in their ability to navigate the complexities of the process. Technological capabilities are also essential, as advanced software systems and automation tools can streamline workflows and improve accuracy.
Compliance with regulatory standards, such as HIPAA, is non-negotiable to protect patient data and maintain legal and ethical practices. Finally, gathering client testimonials and references provides insight into the outsourcing company’s reputation and the level of satisfaction among their existing clients. By carefully evaluating these factors, healthcare organizations can choose the best prior authorization company to partner with for a seamless and successful outsourcing experience.
Successfully outsourcing prior authorization requires careful planning and collaboration between the healthcare organization and the chosen outsourcing company. To streamline the process, clear communication channels must be established to ensure seamless information exchange and timely updates. Data transfer protocols, including secure electronic methods for sharing patient information and medical records, should be implemented to maintain confidentiality and compliance.
Ongoing collaboration is crucial, with regular meetings and feedback sessions to address any issues or concerns. Additionally, defining roles and responsibilities, setting performance metrics, and establishing service level agreements (SLAs) help maintain accountability and ensure quality outcomes. By proactively managing the outsourcing process, healthcare organizations can maximize the benefits of outsourcing prior authorization and achieve a smooth and efficient transition.
Monitoring and Continuous Improvement:
Once the prior authorization process has been outsourced, it is important for healthcare organizations to implement monitoring mechanisms and continuous improvement initiatives. Regularly tracking key performance indicators (KPIs) such as approval rates, turnaround times, and denial rates allows for the identification of any bottlenecks or areas for improvement. By analysing these metrics, healthcare organizations can collaborate with the outsourcing company to implement corrective measures and optimize the process further.
Ongoing communication and feedback loops facilitate the sharing of insights and best practices, fostering a culture of continuous improvement. This iterative approach ensures that the outsourcing partnership remains dynamic, adaptive, and aligned with evolving industry requirements. Regular audits and compliance check also play a vital role in maintaining quality and adherence to regulatory standards. By proactively monitoring and improving the offshored prior authorization process, healthcare organizations can achieve long-term success and deliver exceptional patient care.
Cost Considerations and Financial Benefits:
When considering outsourcing prior authorization, healthcare organizations should carefully evaluate the financial implications and potential cost savings. While there may be upfront costs associated with partnering with a prior authorization company, the long-term benefits often outweigh the initial investment. Outsourcing eliminates the need for additional staff, training, and infrastructure expenses, resulting in significant cost reductions. Moreover, by streamlining the prior authorization process and increasing approval rates, healthcare organizations can minimize revenue loss due to denials and delays.
Faster approval times also mean expedited patient care and increased patient satisfaction, which can lead to improved patient retention and referrals. By carefully assessing the financial considerations and understanding the potential savings and revenue generation opportunities, healthcare organizations can make informed decisions about outsourcing prior authorization services.
Flexibility and Scalability:
One of the key advantages of outsourcing prior authorization is the flexibility and scalability it offers to healthcare organizations. As patient volumes fluctuate or new services are introduced, the outsourcing partner can quickly adjust resources to accommodate changing needs. This flexibility ensures that prior authorization services can be efficiently scaled up or down based on demand, without the need for significant internal restructuring or hiring.
Additionally, outsourcing allows healthcare organizations to tap into the expertise and resources of the outsourcing company, which can adapt to evolving industry trends and regulatory changes. This adaptability ensures that the prior authorization process remains efficient and compliant, regardless of external factors.
Focus on Core Competencies:
Outsourcing the prior authorization process enables healthcare organizations to refocus their internal resources and expertise on their core competencies. By offloading the administrative burden of prior authorization, healthcare providers can redirect their attention to delivering quality patient care. It also enables providers to devote more time and attention to other critical tasks, such as physician-patient interactions and care coordination.
Enhanced Data Security and Compliance:
Outsourcing prior authorization can provide healthcare organizations with enhanced data security and compliance measures. Reputable outsourcing companies like Promantra prioritizes data protection and invests in robust security protocols to safeguard sensitive patient information. We adhere to industry best practices and comply with stringent regulatory requirements, such as the Health Insurance Portability and Accountability Act (HIPAA).
Promantra is the ideal destination for healthcare organizations to outsource prior authorization process. With their extensive experience and expertise in healthcare revenue cycle management, Promantra offers tailored solutions that streamline the prior authorization workflow, increase approval rates, and reduce denials. Our commitment to data security, compliance, and continuous improvement makes them a trusted partner for healthcare providers seeking efficient and reliable outsourcing services and there by transforming their Prior Authorization process from Chaos to Cashflow.
Contact Promantra today for all you Prior Authorization needs.