
Medical coding is a crucial aspect of the healthcare industry, serving as the backbone of the billing process.
At its core, medical coding involves the transformation of healthcare diagnoses, procedures, medical services, and equipment into universal medical alphanumeric codes. These codes are taken from medical record documentation, such as physician’s notes, laboratory and radiologic results, and more.
The importance of medical coding in healthcare cannot be overstated. Accurate medical coding ensures that healthcare providers are properly reimbursed for their services. It also facilitates efficient and accurate medical billing, helping to streamline the payment process between insurers and providers.
Moreover, medical coding plays a vital role in maintaining comprehensive health records, enabling better patient care and management.
By converting complex medical data into standardized codes, medical coding helps in various administrative functions, including public health reporting, clinical research, and decision-making processes.
In essence, medical coding is indispensable for the seamless operation of the healthcare system, ensuring that every medical service is precisely recorded and billed.
Medical coding translates healthcare diagnoses, procedures, services, and equipment into standardized codes.
These codes are derived from a variety of classification systems such as the International Classification of Diseases (ICD), Current Procedural Terminology (CPT), and the Healthcare Common Procedure Coding System (HCPCS).
Each code set serves a distinct purpose: ICD codes represent diagnoses, CPT codes describe medical procedures and services, and HCPCS codes cover products, supplies, and services not included in the CPT codes.
The process of medical coding begins when a patient visits a healthcare provider. The healthcare professional documents the encounter, including symptoms, diagnoses, procedures performed, and any other relevant information. Medical coders then review these records and assign the appropriate codes to each element of the visit.
For instance, if a patient visits a doctor with flu-like symptoms, the physician’s diagnosis of influenza will be coded using the ICD system.
If the doctor performs a flu test, this procedure will be coded using the CPT system. Each piece of information is thus converted into a precise code that communicates detailed clinical information succinctly and universally.
Medical coders must have a thorough understanding of anatomy, physiology, and medical terminology to accurately interpret patient records and assign the correct codes. They also need to stay updated with the latest coding guidelines and regulations, as these can frequently change.
Medical coders play a pivotal role in the healthcare system. They ensure that the medical services provided are accurately translated into standardized codes, which is essential for billing and reimbursement purposes.
Without accurate coding, healthcare providers would face significant challenges in receiving payment for their services.
Beyond billing, medical coders contribute to the overall efficiency and functionality of the healthcare system. Their work supports various administrative and clinical functions, such as:

Medical coders are essential for translating complex medical information into standardized codes that support the financial, administrative, and clinical operations of the healthcare system. Their expertise ensures that healthcare providers can focus on delivering high-quality patient care while maintaining the necessary administrative accuracy and compliance.
The origin of medical coding can be traced back to the 17th century when the London Bills of Mortality were introduced to monitor deaths from the plague. This early system of classification laid the groundwork for the more systematic approach to categorizing diseases and health conditions.
The modern concept of medical coding began to take shape in the early 20th century with the introduction of the International Classification of Diseases (ICD). The first edition of ICD was adopted in 1893, known then as the International List of Causes of Death. It was developed by Dr. Jacques Bertillon, a French physician, and was primarily used for mortality statistics.
As the healthcare field evolved, so did the need for a more comprehensive and standardized system of medical classification. The ICD system underwent numerous revisions to improve accuracy and reflect advances in medical knowledge. The World Health Organization (WHO) took over the responsibility for the ICD in 1948, further refining and expanding it to encompass a wider range of health conditions and diseases.
In the 1960s, the American Medical Association (AMA) introduced the Current Procedural Terminology (CPT) system to standardize the coding of medical procedures and services. The CPT codes facilitated more efficient billing and reimbursement processes, particularly as healthcare delivery became more complex.
The Healthcare Common Procedure Coding System (HCPCS) was introduced in the 1980s by the Centers for Medicare & Medicaid Services (CMS) to cover products, supplies, and services not included in the CPT codes. These systems collectively provided a robust framework for medical coding that continues to evolve today.
Today, medical coding is more crucial than ever in the healthcare industry. It underpins the entire billing process, ensuring that healthcare providers are accurately compensated for their services.
The precision of medical coding directly impacts the financial health of medical practices and institutions, as well as the timeliness and accuracy of patient billing.
In the modern era, medical coding also plays a significant role in public health and medical research. The data derived from coded health records are invaluable for tracking disease outbreaks, conducting clinical research, and developing health policies. Accurate coding is essential for the collection of reliable health statistics, which are critical for informed decision-making and resource allocation.
Moreover, with the rise of electronic health records (EHRs) and the increasing complexity of healthcare services, the demand for skilled medical coders has grown.
Medical coding ensures that patient records are comprehensive and easily accessible, facilitating better patient care and coordination among healthcare providers.
The history of medical coding reflects its evolution from a rudimentary system of tracking mortality to a sophisticated and essential component of modern healthcare.
Its development has paralleled advances in medical science and technology, and its importance continues to grow in ensuring the efficiency, accuracy, and integrity of healthcare delivery and administration.
Medical coding plays a vital role in the standardization of patient information. By converting complex medical data into universal codes, medical coding ensures that healthcare information is consistently recorded and understood across different systems and providers.
This standardization allows for clear communication among healthcare professionals, reducing misunderstandings and discrepancies in patient records. It also enables the efficient organization and retrieval of patient data, which is essential for maintaining comprehensive and accurate health records.
One of the primary functions of medical coding is to ensure accurate billing and reimbursement. Medical coders translate the healthcare services provided into standardized codes that are used by insurance companies to process claims.
Accurate coding is crucial for healthcare providers to receive appropriate payment for their services. Errors in coding can lead to denied or delayed claims, resulting in financial losses for healthcare providers and potential complications for patients.
By ensuring precise and correct coding, medical coders help streamline the billing process, ensuring that healthcare providers are compensated fairly and promptly.
Medical coding significantly contributes to improving patient care and reducing errors. Accurate coding provides a detailed and precise record of a patient’s medical history, diagnoses, and treatments.
This comprehensive documentation allows healthcare providers to make informed decisions about patient care, leading to better treatment outcomes. Moreover, standardized codes reduce the risk of errors in interpreting medical records, which can occur with free-text descriptions. This accuracy is critical for preventing medical errors, ensuring patient safety, and providing high-quality care.
Efficient data sharing among healthcare providers is another key benefit of medical coding. In today’s interconnected healthcare environment, patients often receive care from multiple providers across different locations.
Standardized medical codes enable seamless sharing of patient information between various healthcare entities, such as hospitals, clinics, and specialists.
This interoperability ensures that all providers have access to the same accurate and up-to-date patient information, facilitating coordinated care and continuity of treatment. It also enhances the efficiency of healthcare delivery by reducing redundant tests and procedures, ultimately improving patient outcomes.
The role of medical coding in the healthcare system is indispensable, supporting both the financial and clinical aspects of healthcare delivery and ultimately contributing to better patient outcomes and a more efficient healthcare system.
Purpose and Usage – The ICD-10-CM is used in the United States to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care. It facilitates the collection and analysis of health information for clinical, administrative, and research purposes. ICD-10-CM is maintained by the National Center for Health Statistics (NCHS) and is used for diagnostic coding.
Overview and Application – The CPT code set, maintained by the American Medical Association (AMA), is used to describe medical, surgical, and diagnostic services. These codes facilitate communication among healthcare providers, patients, and insurers, ensuring that services are billed correctly and efficiently.
Description and Use Cases – HCPCS Level II codes are used to identify products, supplies, and services not included in the CPT codes, such as durable medical equipment, prosthetics, ambulance services, and certain drugs and medications. These codes are maintained by the Centers for Medicare & Medicaid Services (CMS).
Importance in Inpatient Settings – The ICD-10-PCS is used in the United States for coding inpatient hospital procedures. It is maintained by the Centers for Medicare & Medicaid Services (CMS) and provides a detailed and standardized system for documenting procedures performed during hospital stays, ensuring comprehensive and precise records.
Usage in Dental Care – The CDT code set, maintained by the American Dental Association (ADA), is used to document dental procedures. It ensures standardized reporting and billing for dental services.
Tracking and Reporting Drugs – The NDC is a unique identifier for medications intended for human use. The NDC serves as a universal product identifier for drugs, facilitating the tracking and reporting of drug usage and ensuring accuracy in dispensing and billing. The codes are maintained by the Food and Drug Administration (FDA).
Purpose and Application – Modifiers are used in conjunction with CPT and HCPCS codes to provide additional information about the performed procedure without changing the definition of the code. They indicate that a service or procedure has been altered in some way, such as being performed on a specific body part or at a different time. Modifiers are essential for accurate billing and coding, as they provide context that affects reimbursement and clinical documentation.
The process of medical coding involves several steps to ensure that healthcare services are accurately documented and billed. Here’s a detailed look at each stage of the medical coding process.
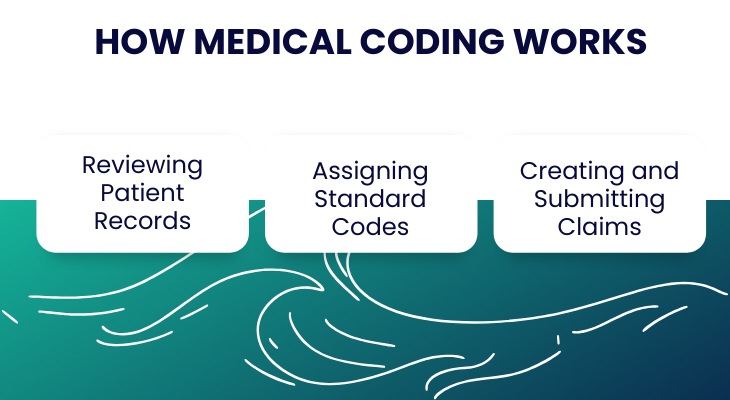
The first step in the medical coding process is reviewing patient records. Medical coders analyze clinical documentation, including physician’s notes, lab reports, radiologic results, and other pertinent information. This comprehensive review ensures that all the medical services provided are captured accurately.
After reviewing the patient records, the medical coder assigns standard codes to each diagnosis, procedure, and service documented.
This involves selecting the appropriate codes from coding systems such as ICD-10-CM for diagnoses, CPT for procedures, and HCPCS for additional services and supplies. The coder must have a deep understanding of medical terminology, anatomy, and coding guidelines to ensure precise code selection.
Once the codes are assigned, the next step is to create and submit claims to insurance companies.
The codes are entered into the healthcare provider’s billing system, generating a claim that includes all the necessary codes along with the patient’s demographic information and details of the healthcare provider. This claim is then submitted electronically to the patient’s insurance company for reimbursement.
Medical coders perform a variety of tasks daily, including:
Consider a patient who visits their doctor complaining of a sore throat and fever. Here’s how a medical coding transaction might unfold:
Let us look at how medical coding is improving healthcare significantly:
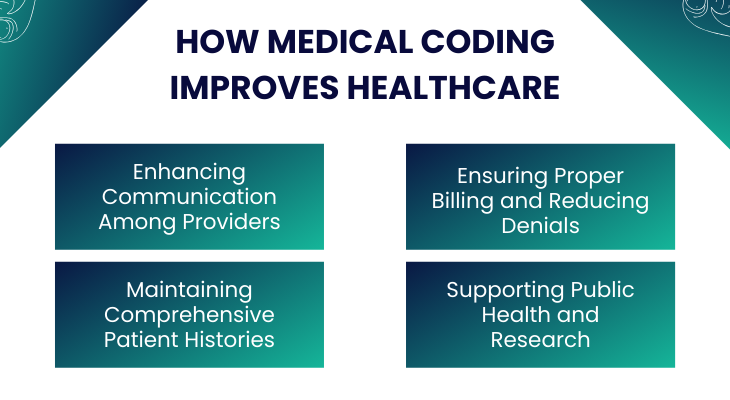
Medical coding significantly enhances communication among healthcare providers by standardizing the language used to describe diagnoses, procedures, and treatments.
This standardization ensures that all healthcare professionals, regardless of their location or specialty, can understand and interpret patient information consistently.
For instance, if a patient is referred from a general practitioner to a specialist, the standardized codes in the patient’s record allow the specialist to quickly grasp the patient’s medical history and current health status. This seamless communication improves the coordination of care, reduces the risk of errors, and ensures that patients receive timely and appropriate treatment.
Accurate medical coding is essential for proper billing and reimbursement. Insurance companies rely on these standardized codes to process claims and determine the amount to reimburse healthcare providers for their services.
By ensuring that each service and procedure is coded correctly, medical coding reduces the likelihood of claim denials due to coding errors or discrepancies.
This not only helps healthcare providers receive timely payments but also minimizes the administrative burden associated with re-submitting claims and resolving billing issues.
Consequently, proper billing and reduced denials lead to a more efficient healthcare system and better financial stability for healthcare providers.
Medical coding contributes to the maintenance of comprehensive and detailed patient histories. Every diagnosis, treatment, and procedure a patient undergoes is translated into standardized codes and recorded in their medical record.
This systematic documentation allows for a complete and accessible patient history, which is crucial for ongoing patient care.
Comprehensive patient records enable healthcare providers to track a patient’s health over time, identify patterns or changes in their condition, and make informed decisions about future care.
Additionally, detailed patient histories improve continuity of care, especially when patients see multiple providers or switch healthcare facilities.
Medical coding plays a vital role in supporting public health initiatives and medical research. The standardized data generated from coded medical records is invaluable for tracking disease outbreaks, identifying health trends, and conducting epidemiological studies.
Public health organizations use this data to monitor the prevalence and incidence of diseases, assess the effectiveness of interventions, and allocate resources efficiently.
Moreover, researchers rely on accurate and comprehensive coded data to conduct clinical trials, develop new treatments, and advance medical knowledge.
By providing reliable and standardized data, medical coding supports evidence-based practices and contributes to the overall improvement of public health and medical research.
Medical coding relies on a variety of tools and systems to ensure accuracy, efficiency, and compliance. This section will discuss the critical role of EHR systems, coding software and databases, and their integration with billing systems.
Electronic Health Records (EHR) systems are digital versions of patients’ paper charts and are fundamental tools in modern medical coding. These systems streamline the documentation process by allowing healthcare providers to enter patient information electronically. EHR systems offer several benefits for medical coders:
Coding software and databases are essential tools for medical coders, helping them navigate complex coding systems and ensure accuracy. These tools include:
Integration with billing systems is crucial for the seamless operation of medical coding and billing processes. This integration offers several advantages:
Implementing best practices in medical coding can significantly enhance accuracy, efficiency, and compliance. This section discusses the importance of integrating coding into healthcare workflows, customizing EHR systems, automating billing processes, and tracking progress through feedback loops.
Integrating coding directly into healthcare workflows ensures that coding is a seamless part of the patient care process. This can be achieved by:
Customizing EHR systems to meet the specific needs of a healthcare facility can greatly improve coding accuracy. This involves:
Automation in billing processes helps reduce administrative workload and improve accuracy. Key practices include:
Tracking the progress of coding and billing activities and creating feedback loops can help identify areas for improvement. Strategies include:
Medical coders face numerous challenges that can impact the accuracy and efficiency of the coding process.
This section highlights common challenges and strategies to overcome them, as well as the importance of continuous education and training.
Continuous education and training are crucial for maintaining high standards in medical coding. This includes:
By implementing these best practices and addressing the challenges through targeted strategies and continuous education, healthcare organizations can improve the accuracy, efficiency, and compliance of their medical coding processes
Medical coding is a critical component of the healthcare system, ensuring that patient information is accurately documented and seamlessly communicated among providers.
By standardizing the language used to describe diagnoses, procedures, and treatments, medical coding enhances the quality of care, supports efficient billing processes, and facilitates comprehensive patient records.
Advanced tools and systems like EHRs, coding software, and integrated billing systems play a pivotal role in making the coding process more accurate and efficient, ultimately contributing to better healthcare outcomes.
Despite the challenges faced by medical coders, including complex coding systems, regulatory compliance, and high workloads, adopting best practices and continuous education can significantly mitigate these issues.
By building coding into healthcare workflows, customizing EHR systems, automating billing processes, and tracking progress, healthcare organizations can ensure that their coding practices remain accurate and compliant.
As medical coding continues to evolve, its importance in improving patient care, supporting public health, and advancing medical research cannot be overstated.
ProMantra has been a reliable partner for healthcare providers across the United States for over two decades. We understand the pivotal role medical coding plays in the financial health of your practice.
Our certified coders bring extensive experience and a passion for accuracy and efficiency, making us an integral part of your team.
We offer a comprehensive suite of medical coding services that go beyond merely assigning codes, helping to enhance your revenue and streamline your workflow.
Our meticulous coding practices ensure that you capture the full value of your services by identifying all billable procedures and diagnoses according to the latest ICD-10-CM and CPT guidelines. This approach significantly boosts your bottom line by increasing and speeding up reimbursements from insurance companies. ProMantra’s certified coders ensure every code accurately reflects the services provided, optimizing your revenue cycle management.
With our deep understanding of coding regulations and attention to detail, we help avoid errors that lead to claim denials and delays. This results in a smoother revenue cycle and steady cash flow for your practice. By reducing errors and improving claim accuracy, we help you avoid the financial disruptions caused by denied or delayed reimbursements.
Our streamlined coding processes free up your valuable time and resources, allowing you to focus on delivering excellent patient care while we handle the complex, behind-the-scenes work of medical coding. ProMantra’s solutions integrate seamlessly with your existing workflows, enhancing overall operational efficiency.
ProMantra’s expertise extends far beyond accurate coding. We are committed to being a strategic partner in your revenue growth journey. Healthcare providers across the United States have experienced an average revenue increase of 30% by implementing our medical coding services.
This financial security allows you to invest in your practice, expand services, and deliver better patient care. We offer a range of services including inpatient and outpatient coding, E/M coding, procedure and diagnosis coding, specialty coding, and coding audits and reviews, all designed to maximize reimbursements and streamline workflows.
By choosing ProMantra for your medical coding services, you gain access to a team of expert and certified medical coders dedicated to delivering accurate, efficient, and compliant coding solutions.
This partnership allows you to concentrate on what truly matters—providing exceptional patient care.
Ready to experience the advantages of partnering with ProMantra for your medical coding needs? We can help you enhance accuracy, boost efficiency, and maximize your reimbursements.
Schedule a Free Consultation today! Our team of experts will assess your specific requirements and answer any questions you may have.
We’ll also provide a tailored proposal detailing how ProMantra can streamline your medical coding processes to enhance your practice’s financial health.
Reach out to us now and take the first step towards a more efficient and profitable healthcare practice with ProMantra.